mypainweb shares with you MY experiences and MY understanding of chronic back pain and surgery.
In no way does this constitute a medical opinion or negate the advice of your personal doctor or surgeon in any way. mypainweb’s intention is to INFORM you of my personal experiences and understanding.
As we all know, no two people are alike and neither are any two surgeries. We know there are risks involved with certain procedures and any surgery. You are best advised by your personal physician and surgeon about what outcome(s) you can hope to achieve. It is in your best interest to be as informed as you possibly can be, before making any decisions, weighing your options against your own personal judgments or belief system.
WHY SURGERY?
Pain alone is NOT the reason for spine surgery. It must be determined that you have an abnormality in your spine and that the abnormality is causing your pain. Here are a few abnormalities that MAY require spine surgery:
1. Scoliosis, a curvature of the spine
2. Kyphosis, a humpback deformity
3. Spondylolisthesis, the forward slippage of a segment of the spine
4. Spinal stenosis, narrowing of the spinal canal typically from arthritis
5. Radiculopathy*, the irritation and inflammation of a nerve caused by a herniated disk
6. Degenerative disc disease, the development of pain in a disc as a result of its normal wear and tear (Spondylosis, Bone Spurs)
Spine surgery is, and for the foreseeable future will remain, a controversial topic. We all know people who have had back surgery that still have problems. Some of you may also know people who have had back surgery that has worked quite well.
Of all people with back and neck pain, experts state that only 2%-5% should ever need surgery. This means that the vast majority of these problems will be successfully treated using non-surgical interventions. There is a common belief among people that if the symptoms are bad enough one can always have surgery. This is simply not true. For most conditions of chronic back and neck pain there is no surgical solution.

Before you decide to have spine surgery or told you need spine surgery YOU MUST listen to the following podcast “Why a Back Surgeon Doesn’t Recommend Back Surgery (for most patients)”:
Click on the following podcast link:
“Why a Back Surgeon Doesn’t Recommend Back Surgery (for most patients)”podcast
Click on the following pdf version of the Dr. Hanscom’s podcast to read his incredible spine surgery straight talk:
Click on the following pdf version:
“Why a Back Surgeon Doesn’t Recommend Back Surgery (for most patients)”pdf
Want to read more?
Click on the following link:
What to read something more extensive? Perhaps with more depth? Click on the following link to read about a study comparing surgical versus non-surgical therapy for chronic low back pain:
Four-year follow-up of surgical versus non-surgical therapy for chronic low back pain
Radiculopathy*:
What You Need to Know….
- Radiculopathy describes a range of symptoms produced by the pinching of a nerve root in the spinal column.
Click on the following John Hopkins Medicine link to understand Radiculopathy:
WHAT SURGERY?
Here are a list of the more prevalent spine surgeries:
1. Discectomy. This involves removal of the herniated portion of a disc to relieve irritation and inflammation of a nerve. It’s done as an open surgery and typically involves full or partial removal of the back portion of a vertebra (lamina) to access the ruptured disk.
2. Laminectomy. This procedure involves the removal of the bone overlying the spinal canal. It enlarges the spinal canal and is performed to relieve nerve pressure caused by spinal stenosis.
3. Fusion. Spinal fusion permanently connects two or more bones in your spine. It can relieve pain by adding stability to a spinal fracture. It is occasionally used to eliminate painful motion between vertebrae that can result from a degenerated or injured disk. Bone grafts with or without instrumentation may be required (hardware consisting of rods, cages, hooks, wires, plates and screws).
4. Vertebroplasty. During this procedure, your surgeon injects bone cement into compressed vertebrae. For fractured and compressed vertebrae, this procedure can help stabilize fractures and relieve pain. With a similar but more expensive procedure — called kyphoplasty — a balloon-like device is inserted to attempt to expand compressed vertebrae before bone cement is injected.
5. Artificial disks. Implanted artificial disks are a treatment alternative to spinal fusion for painful movement between two vertebrae due to a degenerated or injured disk. These relatively new devices are still being studied, however, so it’s not yet clear what role they might play as a back surgery option.
The surgery itself can be performed using a number of various techniques:
- Invasive Surgery: A form of surgery that involves making an incision in the patient’s body and inserting instruments or other medical devices into it.
- Minimally Invasive Surgery (MIS): MIS was developed to treat disorders with less disruption to the muscles. This can result in quicker recovery, decreased operative blood loss, and helping to speed patient return to normal function. In some MIS approaches, also called “keyhole surgeries,” surgeons use a tiny endoscope with a camera on the end, which is inserted through a small incision in the skin. The camera provides surgeons with an inside view, enabling surgical access to the affected area of the spine.
- Continual diagnostic procedures advances may be used during surgery including:
- Laparoscopy: A minimally-invasive surgical or diagnostic procedure that uses a flexible endoscope (laparoscope)
- Laser: Laser (light amplification by stimulated emission of radiation) surgery uses an intensely hot, precisely focused beam of light to remove or vaporize tissue and control bleeding
- Robotic: the performance of operative procedures with the assistance of robotic technology. It allows great precision and is used for remote-control, minimally invasive procedures.
WHO PERFORMS THE SURGERY?
A neurosurgeon or an orthopedic surgeon? It’s your choice. Both
neurosurgeons and orthopedic surgeons perform spine surgery.
Currently, neurosurgeons seek board certification from the American Board of Neurological Surgery and orthopedic surgeons seek certification from the American Board of Orthopedic Surgery.
It is very important that patients make sure that their doctor is certified by the appropriate board. This ensures that the doctor has met the highest standards set by his or her peers and passed both oral and written examinations. Click on mypainweb “Doctor Finder” to help you determine certifications.
Don’t be afraid to ask your surgeon about his or her training, practice focus, experience with whatever operation has been recommended, and whether you, the patient, have been presented with all of the options that exist (regardless of whether your surgeon performs all of them or not). Don’t be afraid to speak up. It’s your body, your spine. Physicians place great value on educating patients to the best of their ability so that satisfactory decisions can be made and acceptable treatment initiated.
Here are a few good questions to ask your surgeon:
- Are you board-certified?
- How many surgeries like this did you do last year, and what were the results?
- Are the results (data) available to patients?
- Do you have a sense of how your patients do who choose surgery vs. those who choose not to have surgery?
- What makes you think that surgery is the right course of action?
- Will anything bad happen if I don’t have surgery?
- May I talk to one of your patients who underwent a similar operation about a year ago?
WHEN SOULD THE SURGERY BE DONE?
Many common back problems–even those that cause severe pain–will resolve themselves over time using “Conservative” therapies and other non-surgical interventions. Patients without associated symptoms in their legs should generally wait a minimum of 6 to 12 weeks.
If there is no improvement, and pain is severe and disabling, spinal surgery may be an option to consider provided you have been properly evaluated by at least one surgeon and a second surgeon to obtain a second opinion.
The inability to control your bladder and/or bowels may indicate a medical emergency requiring immediate medical attention.
It’s important that all “Conservative” therapies and other non-surgical interventions were properly used and trialled prior to surgery consideration.
Lastly, you must clearly understand the risks and benefits of the proposed treatment options.
RISKS AND COMPLICATIONS:
Complications from spine surgery are not infrequent. The following websites provide a detailed list of the risks and complications:
Back Surgery that Does Not Relieve Back Pain
Medical errors are an inherent risk of any invasive surgical procedure. Being cognizant of this will help you minimize this risk by understanding, questioning, and clarifying.
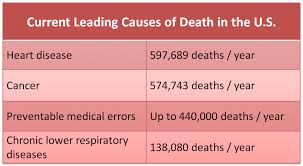
Medical errors are more common than you think. If medical errors were a disease, they would be the sixth leading cause of death in America.
Here are a few medical error statistics:
- *Medical errors kill the equivalent of four jumbo jets’ worth of passengers every week, but the death toll is being largely ignored
- *It’s estimated that up to 30 percent of all medical procedures, tests and medications may be unnecessary — at a cost of at least $210 billion a year (plus the untold cost of emotional suffering and related complications and even death — which are impossible to put numbers on)
- *Urgent reforms are needed to make medical care safer, and simple steps, like installing cameras in hospitals and making hospital performance / error data public, could have a dramatic effect on patient safety
According to the 2011 Health Grades Hospital Quality in America Study, the incidence rate of medical harm occurring in the United States is estimated to be over 40,000 harmful and/or lethal medical errors each and EVERY day.
The following link discusses this disturbing trend along with helpful tips to help keep you safe:
mypainweb “Links” contains more links for reference..
KEEP IN MIND….
Before you agree to back surgery, get a second opinion from another qualified spine specialist. Spine surgeons hold differing opinions about when to operate, what type of surgery to perform, and whether surgery — for some spine conditions — is warranted at all.
Diagnosing and treating back and leg pain can be a complex issue, which may require a team of health professionals to diagnose and treat.
SURGERY :
- may be the last resort to help reduce your chronic pain, but there is no guarantee that surgery will reduce your pain.
- is controversial with significant risks and complications. It’s possible your post-surgical chronic pain may be worse than before surgery.
- is NOT a substitute for “Conservative” therapies and other non-surgical interventions. All non-surgical options must be properly used and trialled prior to surgery.
- is considered the point of no return; meaning most surgical interventions are permanent.
MY PERSONAL DECISION:
I asked my doctor if I was a candidate for either a spinal cord stimulator and /or an intrathecal pump. Both of these advanced pain therapy devices are easily implanted beneath the skin:
Spinal Cord Stimulator:
Spinal cord stimulation (also known as neurostimulation therapy) is delivered by way of a small electronic device called a spinal cord stimulator (similar to a pacemaker) surgically implanted under the skin. It delivers mild electrical impulses to your spine, causing a tingling sensation in the area of your chronic pain. Instead of feeling pain, you feel a tingling sensation.
Intrathecal Pump:
Intrathecal pumps (also called “intrathecal drug delivery systems”) deliver pain medication directly to the fluid around the spinal cord. This may result in more effective pain relief with fewer side effects than oral medication, which must first be digested, then passed through the circulatory system with absorption in the brain to reduce pain, thus effecting all systems.
Both of these implanted devices are effective in reducing chronic pain. It does take patient understanding and patience to continually work with these devices to maximize their benefits.
While these devices are safe and proven effective, they will from time to time require your active participation. The power source for these electronic devices are located within the implanted device. The power source is a battery. The device manufacturer for my devices quote a lifespan of about 9 years. Once the lifespan is reached, your surgeon will replace the old device for a new one.
These devices require programming from your doctor along with patient controllers you will use to maximize pain relief from these devices. Intrathecal pumps may be challenging at times as you may need to trial a number of pain medications until you settle on the one(s) which work best for you. Intrathecal pumps use small catheters (tubes) which deliver the medication from the intrathecal pump to the area of injury. These catheters may require surgical fine tuning in the event they should migrate (move) or become blocked. Finally, these devices require frequent monitoring, so you will have regularly scheduled appointments with your Doctor to refill your intrathecal pump as well as adjust medication flow rates. Spinal Cord Stimulators will also require periodic adjustment appointments to insure you are experiencing acceptable pain relief.
Another advantage to the spinal cord stimulator and intrathecal pump implant devices is that both procedures are reversible. In the event the implanted devices are no longer needed or desired, they can be removed surgically.
Please see mypainweb “Timeline” to view my personal experience in using both the spinal cord stimulator and intrathecal pump. The technology is fairly new and is being improved every year to make the devices easier to use, more reliable and more effective. Click on the following website or visitmypainweb “Links” to learn more about these advanced pain therapies:
Of particular note is the fact that an intrathecal pump uses only a fraction of the medication which one would normally require in order to get the same pain relief using oral pain relief medication(s).
The benefit is very little-to-no side effects from this small amount of pain medication delivered from an intrathecal pump. Intrathecal pumps can be programmed to increase or decrease pain medication delivery based upon your pain cycles. New intrathecal pumps are equipped with a PTM (patient therapy manager). This is a hand-held, patient-controlled device allowing the patient to give a pain medication bolus (increase) as needed. This is another benefit, as it helps to further decrease the amount of oral pain medications needed for breakthrough pain.
Your doctor will work with you to determine the best intrathecal pump medication or combination of medications to give you the best pain relief. There is a wide range of intrathecal pump medications used including opioids (morphine, dilaudid) and non-opioids (bupivicaine, baclofen).
Newer intrathecal pump medications like Prialt (ziconotide) are currently being developed and used. Prialt is a new, powerful, non-opioid pain medication that is synthetically produced from the poisonous venom from the Conus Magnus snail. It is highly controversial due to serious physical and psychological side effects. I personally discontinued Prialt therapy after using it for almost two years due to intense side affects. Please visit the following website below to learn more about Prialt side affects: Prialt side effects.
I do not recommend Prialt under any circumstances.
ON A FINAL NOTE…
These devices will not work for everyone. Specific patient selection criteria along with various “trial” techniques are used to help determine if one or both of these devices will provide pain relief.
UPDATE: Intrathecal Pump Therapy…..mypainweb’s personal experience
mypainweb shares with you all aspects of my almost 20 year journey with Chronic Pain. Even the most difficult & frustrating “strands” within mypainweb are revealed to help you understand and take control of your own painweb. One such difficult “strand” was the decision for the removal of my intrathecal pump.
On May 8, 2014 I underwent the surgical procedure to have my intrathecal pump removed. I continued to waffle on this tough decision for 17 months. Multiple times though out each and every day, I agonized over the dilemma of either keeping or having my intrathecal pump removed.
Why decide on intrathecal pump therapy?
Intrathecal pumps are amazing, technically advanced implanted medical devices. If you would like more information about intrathecal pumps click on the following link: mypainweb/invasive surgery.
In practice, an intrathecal pump delivers a preprogrammed, continuous flow of potent opioid pain medication at a fraction of the usual therapeutic oral dosages of opioid pain medications. This has significant advantages. The patient experiences greater reliable pain relief without the usual unwanted and potentially dangerous side affects associated with long term oral opioid pain management therapy. Many people do not tolerate long term high dosages of oral opioids very well. This is what makes intrathecal pump therapy so appealing in managing Chronic Pain. While the intrathecal implanted pump is simple in theory, they do possess a long list of potential complications.
What did I do?
Due diligence. I spent a lot of time researching these neuromodulation implanted medical devices prior to agreeing with my pain physician’s suggestion that I would benefit from an intrathecal pump. I was confident that the benefits of the implanted intrathecal pump far outweighed their reported potential risks.
Interestingly, patients must meet specific selection criteria to receive an intrathecal pump. In addition to meeting certain physical conditions, the patient must also undergo detailed psychological screening prior to intrathecal pump implant surgery.
In the beginning…..
My first intrathecal pump was implanted in February, 2002. My initial period with my intrathecal pump, like many first time intrathecal pump patient’s report, was filled with lackluster results and frustration. Allergic reaction to some of the intrathecal pain medications, migrating catheter tip and improper catheter placement resulted in necessary further surgical revision procedures were some areas of frustration. There must be open communication and close teamwork between the pain physician and patient to effectively coordinate the intrathecal pump pain medication(s).
Getting used to the routine……
Trialling and adjusting the concentration & flow rate of the intrathecal medication, or combination of more than one intrathecal medication within the pump can take several weeks to several months to tweak. Lastly, the periodic “pump fills” must be scheduled as, overtime, the pump’s reservoir must be refilled with medication(s). How does the pump medication(s) get into the implanted intrathecal pump? A manual procedure done by the pain physician involves careful removal of excess medication from the intrathecal pump’s reservoir using a needle placed through the abdomen directly into a port located on the intrathecal pump. Once the excess medication is removed from the intrathecal pump, the pain physician then carefully fills the pump though the needle with a new batch of intrathecal medication. This pump refill process is repeated approximately every 4 weeks to every few months or longer. Pump refill frequency is dependent upon type of intrathecal pump medication(s) used and delivery flow rate of intrathecal medication. As you surmise, these are not medical devices that once they are implanted you can forget about it. On the contrary, a significant commitment on behalf of the the pain physician and the patient are required to achieve success. A high level of confidence in the safety and reliability of the implanted intrathecal pump is also a prerequisite.
Things that made me go hmmmm…..
Given the high-tech, mechanical nature of intrathecal pumps, they are prone to occasional performance problems. One of my earlier pumps was confirmed as being one of the intrathecal pumps on Medtronic’s recall list for battery related performance issues. That particular intrathecal pump had to be replaced in year 3 despite a normal end of life cycle typically lasting 7-9 years.
In and around the aforementioned issues, I’ll be the first to say “they do work”. I did experience periods of times when the intrathecal pump provided the expected adequate pain relief where all that was required was the usual pump refill appointments along with necessary follow up visits to adjust intrathecal pump flow rates.
An added feature called a PTM (Personal Therapy Manager) made the intrathecal pump even more effective. The PTM is a patient handheld device allowing the patient to give themselves a bolus (increase in intrathecal pump pain medication). During times of breakthrough pain, the PTM would offer patients greater control over their pain by giving themselves a bolus. Bolus parameters are preset by the pain physician.
One of my biggest fears realized……
The concern for my personal safety occurred during December 2012. During the week of December 8, 2012 my intrathecal pump , without warning, experienced a serious device-related performance problem resulting in pain medication over-infusion. I experienced this episode not once, but twice in the same week. The over-infusion of pain medication side affects created a medical emergency on both occasions requiring emergency medical treatment.
The side effects I experienced from the over-infusion of pain medication was swift and potentially life threatening. Within just a few minutes I was completely numb from my chest to my toes. No feeling. No sensation. Unable to move. Panic then set in as I found myself having great difficulty in just taking a breath. As previously mentioned, this episode happened on two separate occasions during the same week of December 8, 2012.
What caused the unexpected over-infusion of pain medication?
Medtronic and the doctors (neurosurgeon and pain doctor) could not provide any reason(s) as to why my intrathecal pump over-infused pain medication on 2 separate occasions during the same week.
My pain doctor thought the problem may have been the result of an error in the compounding of my intrathecal pump pain medications. The combination of intrathecal pain medications that I required is manually compounded at a pharmaceutical lab. It was probable that human error was the culprit when my batch of intrathecal pain medication was formulated. As a result, my pain doctor quickly removed the remaining intrathecal pump medications from my pump and sent it out to be tested by an independent lab. The independent lab test results came back normal.
Ultimately, the problematic intrathecal pump was explanted and tested by Medtronic. The intrathecal pump was found, according to Medtronic’s findings, to be operating “normally”.
The general consensus was that it was an “anomaly”. I was told such an occurrence was “unheard of”. I remained cautiously optimistic agreeing to having a new pump implanted.
Confidence shaken to the core….
Even after this new pump was implanted, I constantly experienced prolonged periods of anxiety caused by an impending feeling that another intrathecal pump malfunction, similar to what I experienced months before, may happen at anytime.
Further complicating this matter was the following media article reporting serious health problems and deaths from the same intrathecal pump as mine. Click on the following link to read more about this report: Medtronic Pain Pump blamed for 14 Deaths.
Medtronic posts ongoing Product Advisory / Recall Notifications on their website. I occasionally reviewed them, but still felt somewhat confident that intrathecal pump benefits outweigh the risks. However; my confidence in the intrathecal pump device technology was shaken from the 2 intrathecal pump over-infusion malfunctions I experienced during December 2012. The following link contains Medtronic Advisory / Recall History: Medtronic Advisory / Recall History
Although the SynchroMed pump , my particular intrathecal pump model, has been classified by the Food and Drug Administration as a Class I recall, meaning there was a “reasonable probability” that it could cause serious health problems or even death, the company (Medtronic) is not recommending that the pump be removed.
A change of heart……
The pendulum swung to the other side clearly indicating to me that the risk of serious health problems and/or death far outweighed the benefits of intrathecal pump pain therapy after I read the following Medtronic Over-infusion Product Advisory on the Medtronic website: Medtronic Over-infusion Product Advisory and Medtronic Over-infusion letter.
While I understand that Medtronic reports an acceptable low incident rate of intrathecal pump malfunction, the odds were too great for me to justify continuation of intrathecal pump pain therapy as I experienced, first-hand, the reported intrathecal pump over-infusion malfunction not once, but twice.
Unfortunately, this latest potential intrathecal pump problem, as self-reported by the device manufacturer, Medtronic, is the last in a series performance/reliability problems during the past few years that pose a real question of risk with this technology. In my mind, and in my personal opinion, this risk, which may result in death, far outweighs the benefit of some pain relief.
Furthermore, this Medtronic Over-infusion Product Advisory confirms my fears which first surfaced some 17 months earlier that the intrathecal pump can experience over-infusion malfunction without warning with tragic outcomes.
I have returned to an oral opioid pain management therapy approach with my pain management doctor along with revisiting & fine tuning the many other Chronic Pain strategies and tactics you will find on mypainweb to help take control of mypainweb and improve some quality of life.
A WORD ABOUT FUSION…
Spinal fusion is a surgical procedure used to correct problems with the small bones of the spine (vertebrae). It is essentially a “welding” process. The basic idea is to fuse together the painful vertebrae so that they heal into a single, solid bone. Instrumentation (hardware) is often implanted in the form of plates, cages and screws to insure a solid fusion.
Spine surgery is usually recommended only when your doctor can pinpoint the source of your pain. To do this, your doctor may use imaging tests, such as x-rays, computed tomography (CT), and magnetic resonance imaging (MRI) scans. Specialized diagnostic procedures may also be done (myelogram and/or discogram) to help determine the need for spinal fusion.
Click on mypainweb “Timeline” to learn about my spinal fusion surgeries.
FBSS (Failed Back Surgery Syndrome):
Failed Back Surgery Syndrome (also called FBSS, or failed back syndrome) is a misnomer, as it is not actually a syndrome – it is a very generalized term that is often used to describe the condition of patients who have not had a successful result with back surgery or spine surgery and have experienced continued pain after surgery. There is no equivalent term for failed back surgery syndrome in any other type of surgery (e.g. there is no failed cardiac surgery syndrome, failed knee surgery syndrome, etc.).
Click on the following websites and mypainweb “Links” to learn more about failed back surgery syndrome: Fusion surgery considerations, Failed Back Surgery, and Failed Back Surgery Syndrome.
Failed Back Surgery Syndrome (FBSS) has been one the most painful and complicated strands within mypainweb. Those who suffer from FBSS face increasing disability as well as continual severe chronic pain.
FBSS has fallen into a no-man’s land between surgery and medicine.
ASD (Adjacent Segment Disease):
If your are seriously considering spinal fusion, you MUST discuss ASD (Adjacent Segment Disease) with your surgeon.
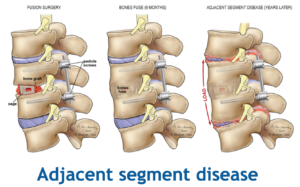
ASD is a potential outcome of spinal fusion. ASD is excessive wear & tear on adjacent non-fused spine segment from the fused level(s) that may result in necessary additional surgery.
Click on the following link to learn more about ASD:
ASD (Adjacent Segment Disease)
WHAT TO DO IF YOU MUST HAVE A SPINAL FUSION
In the event you should find yourself with more than one qualified surgical opinion recommending spinal fusion surgery, I would pursue the Anterior Lumbar Interbody Fusion. The following website below will explain this spinal fusion procedure: Anterior Lumbar Interbody Fusion.
In the case of a cervical (neck) spinal fusion, a surgical procedure called ACDF (Anterior Cervical Discectomy Fusion) is preferred. The following website below will explain this spinal fusion procedure: Anterior Cervical Discectomy Fusion.
While we have made advances in treating spine related chronic pain from the early days (as noted in this picture below), chronic pain remains a mystery, evidenced by epidemic growth in people living with chronic pain even after surgical intervention.
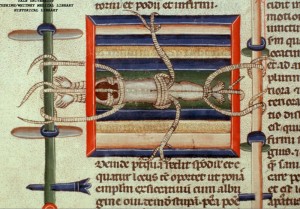
This an an Italian painting (circa 1300?) from an unknown artist from Italy.
The patient is roped to a stretching frame to reduce (correct) a dislocation. The patient is lying face-down with head towards the left, and feet to the right. Ropes go from the arms, head and shoulders to the post on the left; around hips to top and bottom parts of the frame and ankles to post on the right.