Controversy and contradiction are found in almost every aspect of chronic pain. It’s so widespread and deeply rooted, that controversy and contradiction are, in of itself, an added strand within the painweb.
While the numbers may vary somewhat based upon who is reporting, it is universally accepted that chronic pain is a major public health problem. According to the National Centers for Health Statistics, chronic pain has reached epidemic proportions.
In 1999 50 million people suffered from chronic pain. Today, in the United States alone that number increased to over 100 million.
There lacks a single, seamless approach to managing chronic pain. While there is no shortage of interventions, with new ones being introduced on an almost daily basis, chronic pain continues to run rampant.
Albert Einstein once said “ Insanity: doing the same thing over and over again and expecting different results.” The repetitive practice of diagnostic testing, of prescribing medications, along with an ever growing menu of surgical procedures does not insure a reduction or elimination of chronic pain. The hope of restoring function and quality of life often falls short of the expected target.
Mutual frustration from both the doctor and chronic pain patient is a common result. Despite expensive interventions, including those recently developed, chronic pain continues at epidemic levels.
Here’s some recent Chronic Pain statistics:
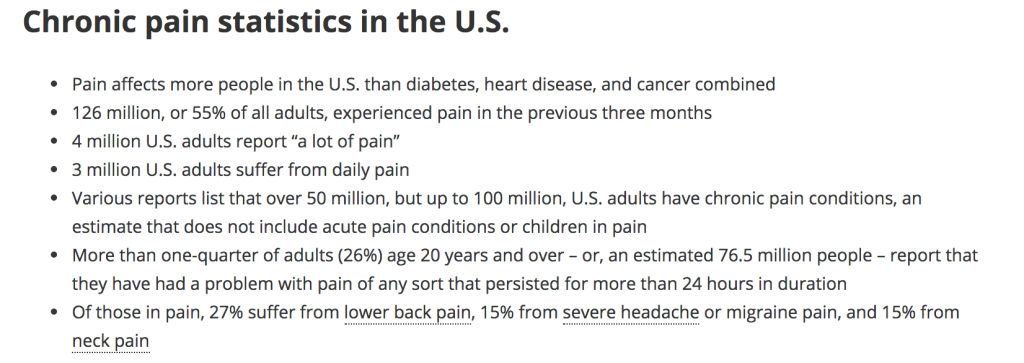
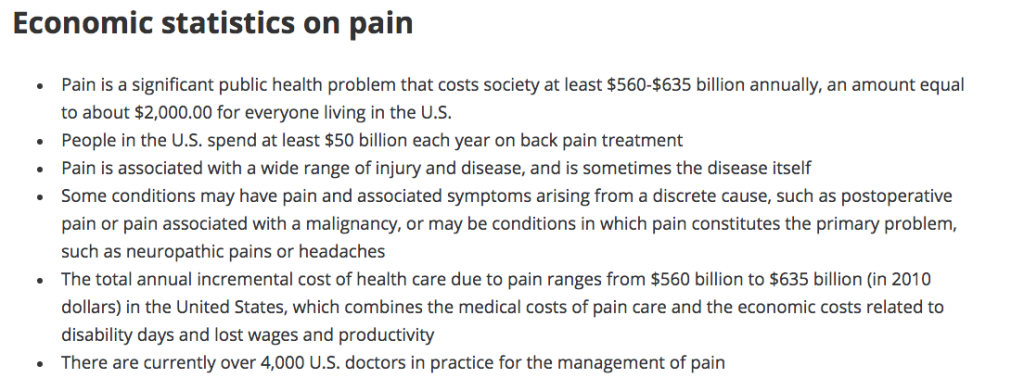

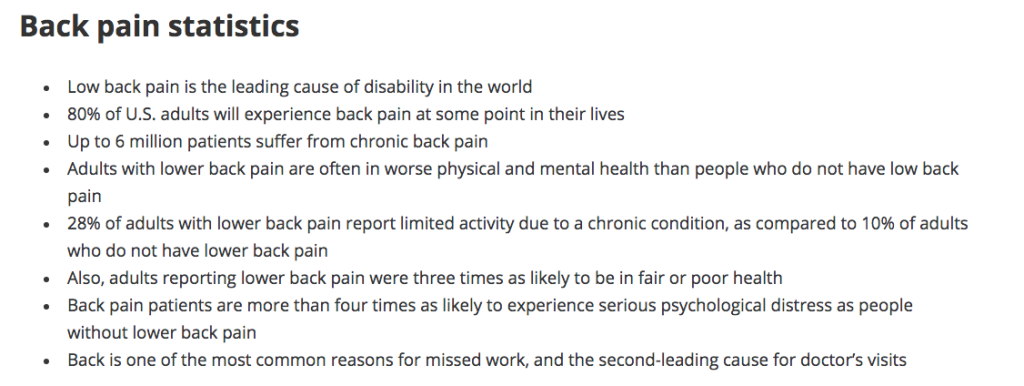
The above chronic pain statistics are taken from the American Academy of Pain Medicine, National Institutes and Health, American Chiropractic Association, and American Society of Addiction Medicine. Thank you Pain Doctor for publishing.
Here are a few more published statistics supporting the growing problematic epidemic of chronic pain:
| ……………………………………………………. | 1993 | 1999 | 2003/4 | 2005/6 | 2009 | 2014 |
|---|---|---|---|---|---|---|
| People with Chronic Pain (millions) | 50 mil | 76 mil | 100 mil | |||
| Work days lost due to Chronic Pain (millions) | 36 mil | 83 mil | 100 mil | |||
| Fusion Surgeries (hundred thousands) | 184 k | 460 k | 500 k | 1.1 mil | ||
| Implant Sales (millions/billions) | $211 mil | $2.5 bil | $25 bil | |||
| People w/ Failed Back Surgery Syndrome (thousands) | 18-72 k | 46-184 k | 110-440k | |||
| Medicare cost for pain disability (billions) | $70 bil | $300 bil | ||||
| Medicare cost in-patient back surgery (millions) | $75 mil | $75 mil |
CONTROVERSY & CONTRADICTION
It’s important to understand that much has been published and debated about the actual existence of chronic pain. There remains much controversy in, and contradiction of chronic pain, in both the actual existence of chronic pain, and the methods used to treat it. The following with website links are just a few examples:
- Why then is spinal fusion so controversial? There appear to be two factors: the high price of the surgery, and the strong ties between the surgeons performing the spinal fusions and the medical device manufacturers that produce thehardware used in the procedure. (Spinal Fusion Controversy)
- Complication rates of spine fusion surgery are 30%-40%, with re-operation rates at 10%-20%. (Spinal Fusion Controversy)
- There is no agreed upon criteria that surgeons must meet in order for a spine fusion surgery to be considered successful. (Spinal Fusion Success Rates)
- Long-term complications of using an autograft bone graft in spine fusion surgery (the iliac crest bone graft harvesting procedure). (Bone graft complications)
- Complications due to implanting instrumentation (hardware like the BAK cages) during spine fusion surgery. (Disc Replacement Surgery)
- One of the most significant risks occurs when the spinal discs either above or below the fusion wear out and become extremely painful. The incidence of this complication, known as adjacent segment disease (ASD), which often requires a re-fusion of the spine to include the newly affected areas, can be as high as 40%. (Spine Surgery Risks)
- There has been a 20-fold increase in lumbar surgical fusion rates among Medicare enrollees from 1992-3 to 2002-3, representing the largest coefficient of variation seen with any surgical procedure. Long term patient follow ups report that up to 50% of patients are not improved and often are worse. (Failed Back Surgery Syndrome)
- Discography remains controversial (invasive radiological study to determine cause / location of spine pain) to determine necessity for spine surgery. (Spine controversy)
- Click on Spinal Operations Soar Despite Drawbacks to learn more.
- 85% of patients who suffer from chronic low back pain cannot be given a precise diagnosis. (Spine controversy)
- Spinal Fusion Surgery leads to worse long-term outcomes….compared to nonsurgical treatment. (Spinal Fusion worse outcomes)
- While physicians agree on many things about spine fusion surgery, there are some areas that lack consensus: The type of bone used, and how many levels should be fused. (Spinal Fusion Surgery Controversy)
- Whether to have back surgery can be a controversial decision, but a new procedure to reverse it may be even more controversial.
- (Back Surgery Reversal Controversy)
- The economic impact of Failed Back Surgery Syndrome. (FBSS Economic Impact)
Expect controversy and contradiction as you seek chronic pain treatment(s). I’ve learned to expect it, thereby removing the element of surprise. This helps me to remain proactive in an effort to reduce / eliminate my chronic pain.
The following link is another excellent source concerning spine surgery controversy: Overtreated: Surgery too often fails for back pain.
I’ve made the effort to understand and learn about my chronic pain causes, diagnosis, prognosis, and treatments. I offer suggestions to my doctor while questioning my doctor’s advice and proposed solutions. The internet is a valuable resource that helps transform a patient into an active partner with their doctor.
This type of cohesive partnership allows me to further take charge of mypainweb while building my confidence and improving my quality of life.
FIX MY PAIN, PLEASE?
If it were that easy, then the numbers of people living in chronic pain would be decreasing. We know that is not the trend.
Following your Doctor’s orders is not enough. Understanding and questioning treatment options with your Doctor creates the empowerment you must have to manage your chronic pain. Chronic pain is different than a heart attack patient who gives themself to their cardiologist, or that of a cancer patient who gives themself to their oncologist.
In most cases we hear of these patient’s improvement and recovery; a return to their lives. We understand there are setbacks and disappointments, but these patients improve over time. Chronic pain is an anomaly. As advances in medical understanding, technology, and procedures increases, patient successful outcomes decreases.
Chronic pain patients can no longer give themselves to their doctor and say “fix me, please?” Chronic pain patients must take charge of their chronic pain, taking the initiative to understand their chronic pain and learn how to partner with their doctor on longterm strategies and solutions.