During the past 6 months I’ve been experiencing significantly worsening pain along with presenting “new” pain.
Below are a few “low-lights”:
♦ I’ve adjusted to being without the intrathecal pump. The trade off of not experiencing the angst of worry associated with the potential of experience continued pump malfunctions is worth not having some inconsistent pain relief from the pump. My Pain Doctor has adjusted the Nucynta pain medication to help…..
♦ Worsening cervical spine pain along with new pain in both knees and right hip began late May/early June. A peculiar deep pain also felt horizontally mid thoracic area (posterior).
♦ Mild Physical Therapy (8 sessions late May through early September), as prescribed by neurosurgeon was done as a follow up to the 2/28/19 ACDF Surgery. PT was cautious to avoid any further injury/setbacks.
♦ Chest pain began late August/early September. Chest pain occurs upon breathing in…when chest expands and during moving. Chest pain location is on my left side and is always present with vary degrees of pain level; affecting sleep as well.
Several doctor visits were done during October with my pain doctor, neurosurgeon, cardiologist, and primary care doctor. The following diagnostic tests were done:
♦ Chest X-rays
♦ Blood Work
♦ EKG
♦ Echocardiogram
♦ CT Scan with Myelogram (injecting contrast) is scheduled for 10/28/19
I make it a practice to be sure the 4 Doctors share all test results/summaries/findings with each other to be sure each doctor has ALL current medical information.
Here’s what I know so far:
♦ Cardiologist has ruled out chest pain of a cardiac nature…huge relief. Cholesterol level is up a little, so a statin has been prescribed for 10mg every-other-day. Echogram shows some heart valve leakage (ongoing from Mitral Valve Prolapse).
♦ Primary Care Doctor concurs with Cardiologist findings. Ruled out a pleuritic condition (lung wall lining inflammation) and pericarditis (chest wall inflammation) as chest pain sources.
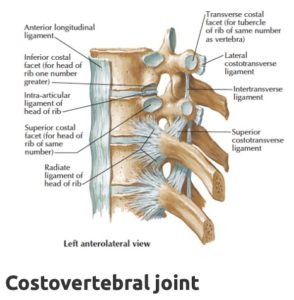
♦ Pain Management doctor confirmed a diagnosis of Fibromyalgia. Also believes chest pain may be from a condition call costochondritis (inflammation of rib cartilage) or costovertebral injury (joint where ribs connect to spine). Both of these musculoskeletal conditions cause the type of chest pain I am experiencing. My chest pain fits closer to a costovertebral injury. A costovertebral injection block will be done on 10/30/19 as a way to give some relief. Relief from injection is indicative of a costovertebral injury.
You can learn more about my Fibromyalgia at the following link: myFibromyalgia.
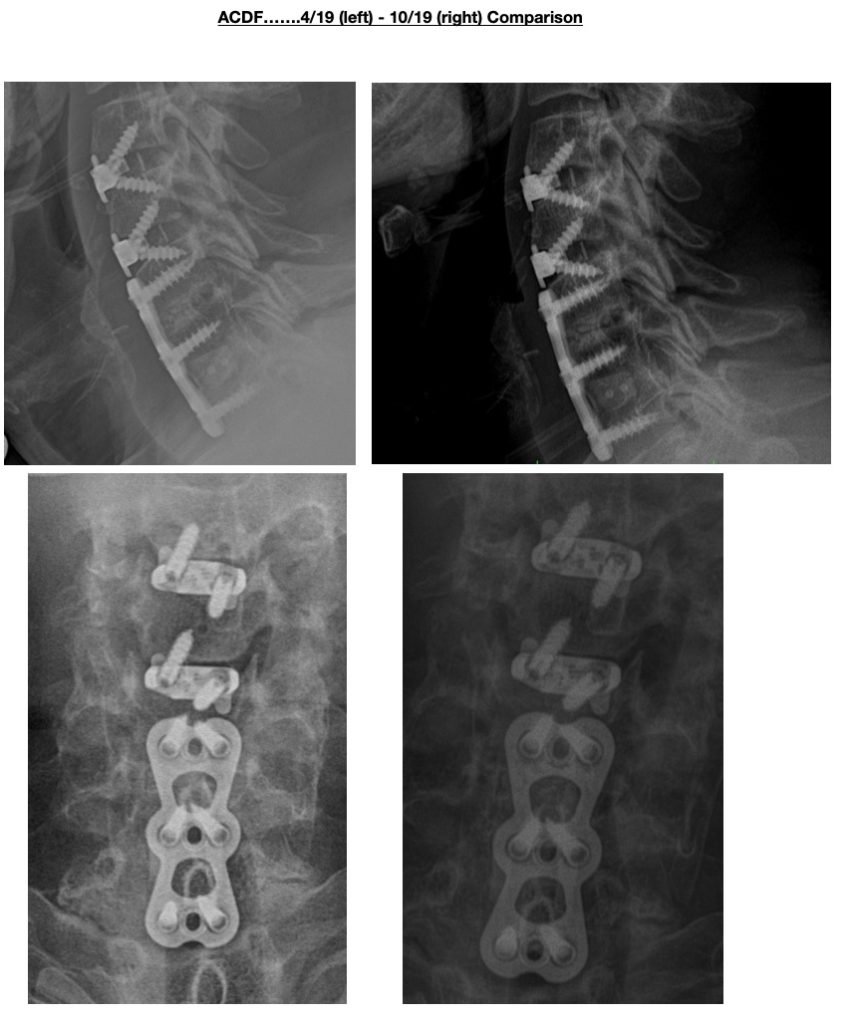
♦ Radiologist Report from 10/19/19 Cervical Spine X-ray notes a possible “Hardware malfunction” from 2/2012 Cervical Spine Fusion. Neurosurgeon doing CT Scan with Myelogram on 10/28/2019. CT w/Myelo will help Neurosurgeon determine what’s causing increasing Cervical Spine Pain with pain radiating to upper back & into fingers.
Below is the comparative X-Ray ….
Here’s an image of costochondritis:
Intrathecal Pump surgically removed today ending 17 years of using intrathecal pumps. Expecting elevated pain during next few days due to post-surgical wound.
Physical Therapy to start after stitches are removed and wound well on its way to heal.
Lastest X-rays (image taken 4/2/19) of Cervical Spine ACDF Surgery (surgery performed 2/28/19.


Hardware alignment good. Bone healing will take approximately 12 months with nerve healing about 24 months.
Decision made to surgically explant (remove) my intrathecal pump on 4/25/19.
Met with Dr. Murphy, a medical marijuana expert/scientist, referred by Dr. Soin, my Pain Management doctor. Dr. Murphy approved me for Medical Marijuana. I will pursue this pain relief option…..
Look for a “coming soon” separate Medical Cannabis section where I will chronicle this pain relief effort on mypainweb.com.
Physical Therapy coordinated; initial consult week of 4/15.
Medical Marijuana. Followed up with State Approved Medical Marijuana Doctor referred by Dr. Soin. Initial Consult on 4/15/19. Medical Marijuana is not covered by insurance. The initial consult with doctor is $200. The required State of Ohio Medical Marijuana ID Card is $50. An appointment or telephone call is required with Doctor every 90 days. Appointment is $100 with the telephone option is $50. Patient choice for appointment or telephone. Only a 13 of the planned 60 State Approved Dispensaries are open. This means very low supply diving up medical marijuana pricing. Currently, pricing per ounce is $200 – $400. An ounce is approximately a month supply of daily use.
C Spine X-rays taken. Healing continuing. X-rays show hardware in proper alignment.
Shoulder/Arm pain improved. OK to stop wearing brace, but move head cautiously. OK to drive.
Will start PT mid April as overall spine & extremities have become weak/atrophied. Next follow up check with Dr. Patel in 6 months.
Healing as expected. Wound closure strips removed. Keep wearing Brace 24-7. Continued restrictions….no cervical extension, flexion or rotation, no lifting over 10 pounds. Next post-op appointment 4/2 for X-rays.
We reached the decision today to discontinue my intrathecal pump therapy after 17 years.
Why?
For me, it’s the cumulative effect of what it takes to insure the best possible outcome from this drug delivery system. I’m one of the patients that experienced the unfortunate Medtronic Pre-mature Battery issues some years back. I also experienced the sudden Medtronic over infusion episodes that created medical emergencies when it occurred not once, but twice a few years ago.
I changed pump manufacturers from Medtronic to Flowonics in 2015. While the Flowonics Prometra II pumps has avoided the Medtronic pump problems, they do have problems too. Add to the above, the complication of insuring the compounding pharmacy get’s the formulation correct for every fill every 3 to 4 months. And….. the “hope” that all the pump programming is done meticulously to avoid errors. Well, it’s been a lot for my brain to manage for the past 17 years. Within this time the pump did provide “some” relief. Never “ complete” relief. And I always experienced “downtime” with increased pain for the many pump related problems I just eluded to. Fast forwarding to the present, the level of relief from my pump no longer outweighs the risks associated with having the pump.
Adding to my own experience is the observation that the numbers of pumps being implanted is dwindling and the technology to make these medical devices safer and more reliable to patients has stalled. We’ve read the difficulties our own pumpsters have experienced from their own pump doctors. Especially from those pumpsters relocating and looking for a new pump doctor. I’m fortunate to have an extremely knowledgable pain doctor that always includes me with his decisions about what’s best for my healthcare.
What will I do?? There’s been some recent radical improvements made within spinal cord stimulation that are being approved by the FDA. These next generation, more powerful devices offer upgrade ability to the patient while they have the capability to “learn” & “react” to our pain. So, these devices become “smarter” over time.. Even better, the upgradability is all software driven…no implanting of newer version devices required.
Another promising opportunity is medical marijuana. Aside for the political “ bologna”, Reports are coming in showing promising results for those with severe chronic pain using the sublingual and/or oral formularies. Worth trying for sure.
Moderate C Spine incision pain. Throat quite painful especially when swallowing. Soft foods preferred. Throat & swallowing difficulty will ease up around 3 weeks post op. Dr. Patel 2 week follow up on 3/19 to include incision check.
Severe lumbar pain with severe quad/hamstring squeezing pain in both legs began 3/11. Dr. Soin said the cervical spine surgery triggered the lumbar-leg pain. Dr. Soin increased oxycontin t0 10 mg from 5mg and also prescribed 2 stronger muscle relaxants: Diazepam & Robaxin. Dr. Soin follow up on 3/18 to refill intrathecal pump and further investigate severe lumbar-leg pain.
Stopped using Diazepam after 2 days; way too strong. Will try the Robaxin in a few days.
Dr. Patel performed an ACDF (Anterior Cervical Decompression fusion) C2-C-5. Previous 2012 ACDF C5-C7 looked fine. Dr. Patel reviewed post op Xray with me; he commented in was a “real mess” that required much work. Surgery lasted approximately 5 hours. C2-C7 are now fused.
What’s ACDF (Anterior Cervical Decompression fusion) surgery?
Good question. This surgery involves accessing the spine through the front of the neck. Posterior Cervical Decompression fusion surgery involves accessing the spine through the back of the neck.
Click on the link below to learn more about ACDF Surgery:
A “bone growth stimulator” has been prescribed; to be worn starting 3/7 for a few months….4 hours each day.
Wait…..Did you say yo have to wear a bone growth stimulator?? Yep.
A bone growth stimulator is a device that stimulate the natural healing process of bone by sending low‑level pulses of electromagnetic energy to the injury or fusion site.

I will need to continue wearing the rigid neck brace….24/7 for 6 weeks.
Below is a picture of the rigid cervical collar prescribed:

Here’s a few notables regarding staying in the hospital:
Pain. Elevated pain levels is to be expected post op. The hospital staff are trained to help keep you comfortable. Removing all pain is not realistic. Reducing pain so you can rest is. A few types of pain medications may be trialled to land on one that you can tolerate. Too much pain medication or requesting too strong pain medication will only complicate your recovery in the hospital. Physical Therapy & Occupational Therapy was started within the first 24 hours of my surgery. Moving, as painful as it may be, is critical as your recovery starts. Too much pain medication can create other medical complications like constipation. Also, your goal should be to reduce pain medication(s) prior to your discharge to help your transition at home a little easier.
Anesthesia. In most cases, several types of anesthesia will be used. The first 24 hours post op may be difficult as your body works to remove the anesthesia from your body. There’s a wide range of anesthesia side affects….the hospital staff will help treat some of them in the event you become ill. You’ll start feeling more like “you” after the first 24 hours.
Drink. Follow all instructions from the Hospital Staff. If you’re cleared to drink, then drink even if you’re not thirsty. This helps to reestablish some balance and to insure everything starts working again without delay.
Instructions. Upon discharge you will receive instructions. Be sure a family member is present to be sure everything is understood in the event you’re not feeling well. Be sure to ask questions to clarify and you understand the at home medication(s) regimen.
Follow up scheduled with Dr. Patel in 2 weeks and then again at 4 weeks post op.

Overall, pain continues to worsen along with greater arm weakness.
All required pre surgery requirements have been met including:
Neurosurgeon consults were done in December & January to discuss symptoms & diagnostic reports.
I selected Dr. Patel, neurosurgeon, with Kettering Brain and Spine. Dr. Patel was knowledgeable and a patient listener. In particular, Dr. Patel was interested in my opinion which he used to help shape his surgical plan.
Surgery set for 2/28/19. Understandable given all that needs to be coordinated for the surgery.
Given my previous 2012 ACDF Surgery, Dr. Patel wants me to see an ENT for a throat scope to clear me for surgery. In addition, I will need to be cleared by my cardiologist for surgery , attend a Spine Fusion Surgery Class and pass a pre-surgery physical. Another reason why time is needed prior to when surgery can be done.
Sudden onset severe pain in neck & left trapezius started 11/17/18.
CT scan below shows C Spine just prior to my 2/12 C Spine surgery (left image) along with C Spine today (middle) and right image showing what a healthy C Spine looks like….
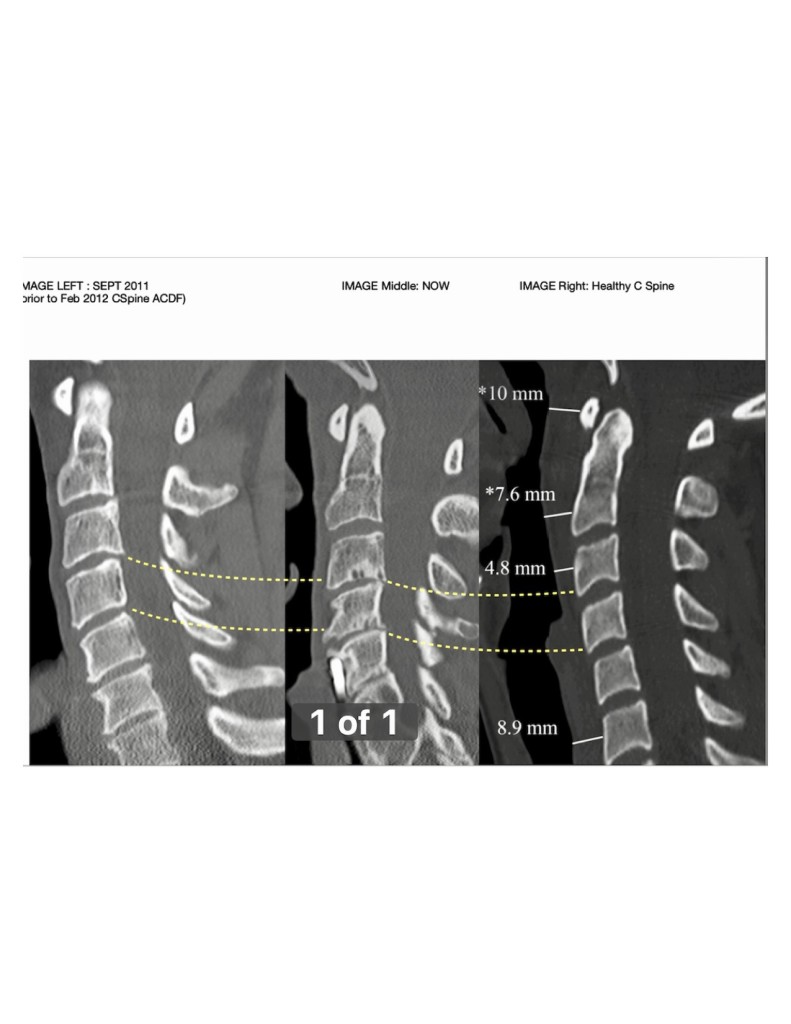
C Spine Radiologist Physician Reports states the following:
C3 – C4:
1) Disc Space Narrowing
2) Facet Arthropathy: pain and discomfort that is caused by degeneration and arthritis of this part of the spine is called facet arthropathy, which simply means a disease or abnormality of the facet joints.
3) Luschka Joint Spurring: Pathological processes that can occur in these joints include degenerative changes or hypertrophic arthritis, resulting in foraminal stenosis and nerve compression. Foraminal stenosis at this joint is the most common cause of cervical nerve root pressure. They were characterized by Hubert von Luschka in 1858.
C4 – C5:
1) Moderate Disc Space Narrowing
2) Endplate Sclerosis & Irregularity: abnormal hardening of body tissue.
3) Facet Arthropathy
4) Vacuum Facet Phenomenon: involves one or more intervertebral discs and can be caused by an accumulation of gas with the disc(s). It usually represents advanced disc degeneration. Since discs are integral to anterior spinal support, vacuum disc is considered to be a sign of instability. In addition, vacuum disc is associated with anterior displacement of a superior vertebral body over the inferior body (spondylolisthesis, spondylolytic spondylolisthesis).
5) Foraminal Stenosis is the narrowing of the cervical disc space caused by enlargement of a joint (the uncinate process) in the spinal canal. Due to facet disease and Luschka Joint Hypertrophy (enlargement).
C5 – C6:
1) Incomplete Bony Bridging
Pain continues to worsen with significant shoulder – arm pain and weakness.
Dr. Soin referred me to a Neurosurgeon to discuss surgical options….December 17, 2018 appointment.
Update to follow…..
Years ago I researched the potential positives of recumbent bicycles for those with chronic back pain. I sourced out one that offered a suspension frame and was eager to try. I recently sold it as it created more pain.
Recently, I read a review of an e-bike (electric bike) written by a chronic pain person with a history of back fusion surgeries. This person provided some details about his spine problems and explained how his e-bike offered some features & benefits that allows him to tolerate riding his e-bike.
What’s an e-bike?? It’s a bike equipped with an electric motor. E-bikes can be ridden with electric power where one doesn’t have to pedal. They also have a pedal assist mode where the electric motor provides power assistance. The rider adjusts the motor power based upon how much, or how little, pedal power they want to use.
I was excited to start researching e-bikes. After spending months learning about them, I thought it was worth a try.
The e-bike model selected by that back fusion patient turned out to be the same model I decided upon. It’s an upright frame, so there’s no leaning posture which is more comfortable for the back. The oversized tires offer a smoother ride. Front suspension helps to absorb bumps and I added a suspension seat post that absorbs bumps that would usually be felt by the spine.
I’m still “trialling” my e-bike. More to follow….
If you’ve spent anytime on mypainweb.com, you know how important staying as active as possible is to managing your pain (physical). Any movement is 1000% better than no movement.
My attempt to sustain exercise in the water was short-lived. Experimenting with modified strokes to minimize trunk rotation and lumbar flexion-extension quickly resulted in significantly worse pain levels. While I’m unable to do it, I give myself credit for trying. Not being afraid to try is important. While I’m disappointed in having to hang up my towel, I will continue to search for another way to keep moving…..
It’s September 2018, so the Prometra II Pump has been in for almost 3 years. Below is a brief of the highlights and lowlights since my last post:
Pump report card….prior to last week I gave it a “B”, but it dropped to a “C-” last week.
The Pump, for the most part, has delivered decent pain relief. As I’ve said, it’s not realistic to expect these devices to completely take away all pain. I’ve been able to discontinue oral pain meds except for a few severe pain flare ups where the pumps bolus feature didn’t help. During those few painful episodes, oral pain meds were needed, but only for a few days. The break-through pain medication I use sparingly is Nucynta. Nucynta is a “mild” opioid. I take the minimum dose of 50 mg.
A pump program error in June of last year caused by the Flowonix Tech created a serious medical problem resulting in complete torso/legs numbness. The Flowonix Tech inadvertently changed the driving drug medication during programming. The mistake was quickly discovered and corrected. However, I experienced some PTSD from that experience which continues, albeit to a lesser degree, today.
A more recent problem surfaced last week (September 2018) where I was experiencing some mild, but bothersome, stomach numbness. Dr. Soin removed all the pump meds from the pump and filled the pump with saline as a way to determine what was causing the numbness. Bupivacaine, a numbing agent, is one of the medications in my pump. Within 5 days…numbness dissipated. No surprise, the pain has been brutal. The oral Nucynta has had a minimal effect on my pain. Dr. Soin refilled pump at 1/2 strength a few days ago. So far, no pain relief.
Dr. Soin is trying to find what’s causing this:
We are considering the following:
Is all this frustrating? You bet. However, this type of advanced pain relief technology is not an “implant it and forget it” strategy. It takes patience and a commitment from both the Doctor and Patient to work through the imminent cycles of ups and downs.
Closing in on 24 weeks post-op….here’s the latest:
Many are asking what does the implant site look like? For those curious…here you go:

This image was taken after a pump refill procedure. The bandaid covers the needle entry point. By the way, the refill procedure is quick and relatively painless.
Comparing the image above with the image below from the 10 week post-op update, you can see the obvious “pump bump” profile from the implanted pump. While the “bump” may appear somewhat large to some, I accept it as a fair trade-off for some pain relief.
Am I all wet? You betcha…..
I explained in my last update that swimming appeared to be my last resort.
Let me properly frame “swimming”….
First, I never liked swimming. Being cold and feeling the wet deck under my bare feet kept me away from pools.
Second, the mechanics of swimming was never my forte; though I could tread water and doggy paddle. Lacking swim technique confidence before starting pool therapy was a real source of angst.
Third, I knew that the few who stare at my pump would cast a shadow of being self-conscious of my appearance.
Fourth, the fear of causing further injury was a huge concern.
I wrote on a sheet of paper the above reasons along with many others supporting why I shouldn’t attempt. The list was long. I thought, no one would argue my reasons for not trying.
But…..these reasons, I knew, were not an excuse for at least giving it a chance.
During the past 3 weeks I went to the pool 2 to 3 times per week.
I set realistic goals of starting off with simple, very movements in the water. I chose just a few of the swimming movements I knew would have minimal effect on my back and neck.
You can click on the following link to review the swimming information I found beneficial:
mypainweb Physical exercise / Swimming
To minimize the possibility of a setback due to straining, twisting, bending, etc, I used the following assistive items:

I use blade fins (above). Helps to keep you buoyant while making kicking motions easier.

These are regular fins (above). This fin would cause too much strain on my back and legs.

Use of a kick board (above) is essential for me. It allows me to stay on top of the water without using my arms.
At some point I would like to use an AquaJogger, pictured below.


“A fish out of water”
While I may look a bit silly in the water, I can hold my head up high for the effort.
My goal is not to swim fast, swim competitively or to look good doing what I’m doing. My goal is to tolerate this activity to continue doing it.
For those that feel they need assistance and help, reach out to your local pool (like a Y). They have staff that can assist you.
Remember, discuss this type of plan with your doctor before you start. By all means, your doctor would be more than happy to authorize a few water therapy sessions with a physical therapist to insure you get started on the right foot…..or, right “fin”.
I’ll be back with my next update soon.
Here are the highlights:
At the 5 month post-op mark, my doctor has titrated the pump’s flow rate a total of 8 times so far. Titration is an adjustment whereby the pump’s continuous flow rate is increased to deliver more medication during a 24 hour perioid.
Overall, the level of pain relief has improved since my 15 Week post-op update. It’s likely we will reduce the frequency of titrations in the coming weeks as the level of intrathecal medication has reached an appropriate, therapeutic level.
The pump” bump” in my abdomen remains larger than what I expected, but given the pain relief, it’s an acceptable trade-off. The throbbing ache from the surgical site is still present when standing / sitting too long, but not as intense at my 15 Week post-op update.
Tolerating the activity:
In follow up to my 15 week post-op update, I carefully chose just a few of the most mild, low impact exercises from the Low Spine Compression program. Click on the following link to learn more about this specific program:
After 3 separate sessions spanning 4 weeks, I discontinued this effort. The onset of severe pain lasting several days after each session was clear feedback that my spine can’t tolerate any weight bearing movements / activities. On a few occasions I was bedridden for a few days; unable to stand or take even a few steps.
It’s important to note that I tried; not once, not twice, but three times. Was I discouraged? Absolutely. However, I realize I have to be realistic and accept amy physical / functional limitations due to my spine injuries & disorders.
What’s next?
Accepting my continued sedentary existence is not an option. With that being said, I created my “new norm”. Something clicked after I read the following urban dictionary definition of “new normal”:
The current state of being after some dramatic change has transpired. What replaces the expected, usual, typical state after an event occurs. The new normal encourages one to deal with current situations rather than lamenting what could have been.
My “new norm” motivated me to keep searching for another option to get myself off the sedentary bench.
Here’s what I found…..
Swimming. That’s right swimming. While I’ve read much about the benefits of swimming, this brief excerpt from a particular swimming rehabilitation article caught my full attention:
There are a few main reasons why swimming is a good rehabilitation tool:
1. It is low impact. (Unless you are training to be an elite swimmer at which point you will be putting your body through a more intense, higher impact workout.)
2. It is a form of active stretching – swimming technically will ensure full range of motion movements for many different body parts.
3. It provides just enough resistance from water to provide, over time, sustained aerobic conditioning to the rehabilitating subject, allowing them to continue to workout while rehabbing at the same time.
Click on the following link to read more about the benefits of swimming for those with Chronic Pain:
mypainweb Physical exercise / Swimming

I’ll report back on my introduction to swimming in my next Prometra II Pump Implant post-op update.
A few observations:
Since my last update, the surgical site has healed. Post-surgical swelling and the “tender-to-the-touch” sensation on the pump and around the surgical site has dissipated.
I notice that standing and sitting for prolonged periods brings on a strong, throbbing ache along with some swelling at the pump implant site. Lying down for a while usually reduces or alleviates the ache.
It appears the “bulge” from the pump (pump bump) will remain somewhat larger than I anticipated. My slightly thicker profile doesn’t concern me in the least as long as I achieve adequate pain relief from my intrathecal pump.
And the Pump:
My doctor has titrated the pump’s flow rate a total of 6 times so far. Titration is an adjustment whereby the pump’s continuous flow rate is increased to deliver more medication during a 24 hour perioid.
The dose of the bolus has also been increased a few times. The Patient Therapy Controller (PTC) is the handheld device that I use to give myself a bolus (short term, temporary increase) of pump medication.
Overall, the level of intrathecal medication is starting to give some pain relief as it reaches a therapeutic level.
What’s next?
In anticipation of reaching this point, some time ago I revisited one of the most important aspects to help me take control of my Chronic Pain. That’s right…..one cannot just sit back. Do nothing and expect the medication to take control. Achieving a quality of life while obtaining some pain relief is the goal. Achieving this goal takes your active role in initiating, maintaining & balancing other key pain management strategies in addition to your effective pain medication strategy.
Revisit the link below to refresh yourself on the other key Chronic Pain relief strategies found on mypainweb:
Sedentary fade-out:
I spent a considerable amount of time researching a safe, low impact exercise program as a means to re-introduce some minimal activity within my life. I came across a very well documented specialized Low Spine Compression program ideal for someone with significant spine limitations and Chronic Pain.
Click on the following link to learn more about the Low Spine Compression program:
mypainweb Physical exercise / Low Spine Compression
My plan is to pick just a few of the most mild, low impact exercises from the Low Spine Compression program to gauge my tolerance and pain levels before, during and after exercising.
I’ll report back my progress in my next Prometra II Pump Implant post-op update.
As I close in on 10 weeks post-op, I thought this would be a good update point.
Pictured below is what the healed surgical site looks like:

My “bulge” profile does take some getting used to. The surgical site continues to heal as bumping the pump does cause some pain. There should be no pain at the surgical site once the area has completely healed.
The neurosurgeon well-placed my pump just above my waistline; avoiding potential discomfort caused by a pressing waistband directly over the pump. Another option for pump placement is in the upper buttocks area. Body type and the pump’s catheter tip location are a few of the variables which determines where best to implant the pump…lower abdominal area like mine, or in the upper buttocks area.
As you can see, you don’t choose to have an intrathecal pump implanted for the “aesthetics”. Achieving Chronic Pain relief is the goal.
Speaking of relief…..the flow rate continues to be slowly titrated up. During the past 10 weeks my Pain Management Doctor has adjusted the flow rate 4 times. Titrating slowly is a safe strategy of increasing the flow rate of the intrathecal medication.
In my case I have a mixture of 2 intrathecal medications. Dilaudid, a strong opioid, is mixed with Bupivacain, an anesthetizing medication. Remember, only a very small amount of intrathecal pump medications are needed to achieve some pain relief. Starting out with a high flow rate and, or titrating aggressively, may result in over-medication side effects. These unwanted over-medication side effects can range from bothersome to dangerous and possibly life-threatening.
Another reason for titrating conservatively is that it usually takes several hours to feel the effects of increasing the pump’s flow rate. This safe slow titrating approach gives ample time to see if any negative side effects develop as a result of a sensitivity or allergic reaction from the pump medication(s).
The goal of achieving pain relief happens when the amount of medication flowing from the pump reaches a therapeutic level. The therapeutic level is different for each patient. I should start feeling some Chronic Pain relief after a few more pump adjustments as the flow rate continues to be slowly increased.
Once I start feeling some Chronic Pain relief, my Pain Management Doctor will know I’m close to my therapeutic level. From here, a few more adjustments will be made to fine-tune the flow rate to maximize therapeutic effects with a minimum amount (minimum flow rate) of pump medication.

I also have been using the PTC (Patient Therapy Controller) on a daily basis. This is the handheld device that I use to give myself a bolus (increase) of pump medication. The goal of the PTC is to provide some relief during those times when Chronic Pain levels spike. Pressing a few buttons on the PTC and then placing the PTC about 1/2 inch directly over my pump will command the pump to deliver a small increase of pump medication. The PTC bolus level is preset and pre-programmed by my Doctor. The PTC also requires a slow, conservative titrating approach. Similar to my pump’s flow rate adjustment, my PTC bolus level is also adjusted. The intrathecal pump and PTC work in tandem to give continuous and “on-demand” Chronic Pain relief.
Communication is critical
As you can see……Communication is critical. Patient-Doctor communication is obvious, but equally important is the communication of Patient-Doctor-Device Manufacturer. The device expert in the room is the technician/representative of the Device Manufacturer. It’s helpful for the patient to establish regular communication with their pump’s manufacturer. This is an effective “check & balance” strategy and a great way to be sure accurate answers are given to specific questions.
Flowonix is the manufacturer of my implanted Prometra II Pump. The Flowonix Technician who assisted the Neurosurgeon in the O.R. during the pump implant surgery has also been present for the follow up pump fill and pump adjustments with my Pain Management Doctor. The collaboration among the three parties (Patient-Doctor-Device Manufacturer) insures we are make the best pump decisions.

In fact, Flowonix takes this relationship, by comparison to other pump manufacturers, to an even better level. A few questions I raised were somewhat involved and complicated. My Flowonix Technician offered me the opportunity to talk directly with a Flowonix engineer. The usual practice would be for the Device Manufacturer Technician to give the best answer, or obtain an answer internally and then call me back with an answer.
Flowonix understands the importance of “delivering” patient confidence. Allowing me to talk directly to a Flowonix Engineer would be a great way to inform and reassure the patient. I can tell you, first-hand, it works. During the past several weeks I had 2 excellent conversations with a Flowonix Engineer. The ample time the engineer took with me to talk on the phone, twice, succeeded not only in answering my questions, but made me feel like an equal partner in managing my healthcare along with my Doctor and Device Manufacturer Technician.
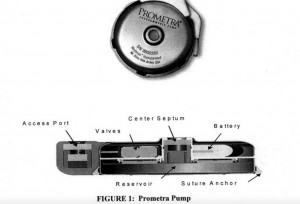
Here a some of the unique safety features of the Prometra II pump I learned from my conversations with the Flowonix Engineer and my Flowonix Technician:

Part of the success of this technology resides with the patient’s willingness to take this type of an active role with their intrathecal pump.
Look for more updates as we continue to adjust flow rates to reach therapeutic levels to feel some relief.
My first pump fill was on October 28, 2015 with my Pain Management Doctor and the Flowonix Tech.
Filling the pump’s reservoir:

The picture above shows how the pump’s reservoir is filled. The pump itself is implanted beneath the skin, so the procedure of filling the pump is a “blind procedure”. Meaning, one “cannot see” the pump. The use of a special needle entering the pump’s reservoir fill port from outside the skin is required to fill the pump. This is a crucial process that requires a highly skilled pain management doctor, or specialized technician to safely access the reservoir fill port. There is no room for error during this procedure as several days, weeks or months worth of powerful pain medication is being delivered into the pump’s reservoir at one time.
The first part of this procedure involves removal of Saline Solution that was used to fill the pump’s reservoir during the 10/12/2015 surgery. The amount of unused Saline Solution removed from the reservoir was accurate given the flow rate of .2000 mg/day while accounting for some Saline Solution remaining in the catheter. This is important as it confirms accuracy of pump’s flow rate.
If you’re interested, you can find below the calculation I used to figure how much Saline Solution should remain to determine the pump’s accuracy :
(a) Saline Solution filled during 10/12 surgery = 19.998ml
16 Days X .2000mg/day = 3.2mg Saline Solution delivered
Catheter Volume = .0896mg (the catheter holds this amount of Saline Solution)
(b) Total amount of Saline Solution delivered = 3.2mg + .0896mg = 3.2896mg
(c) Subtract (b) from (a) to determine unused amount of Saline Solution= 16.7084mg
The calculation determined in (c) should = the actual amount of Saline Solution removed from the reservoir.
A collection tube is used to withdraw the Saline Solution from the pump’s reservoir. The amount of Saline Solution that was physically collected in the tube was spot on with calculation (c) above confirming the accuracy of the Promtetra II delivery system.
The intrathecal pump reservoir is filled with a solution of dilaudid (hydromorphone), an opioid, and buipvacanine, an anesthetic.
Titrating will be done slowly over the next several weeks. This will give my body time to adjust gradually to the pump medications while my doctor and I become familiar with the new Prometra II pump technology.
We will meet next week to increase titration; adding a constant flow rate and increase the bolus rate. The bolus is an increase in medication I control through the use of a handheld patient therapy control device. My doctor presets the bolus flow rate and how many boluses I can administer with a 24 hour period.

Patient Therapy Controller
I will continue the oral Nucynta pain medication as I won’t experience pain relief from the initial low pump medication flow rate. The oral Nucynta pain medication will be tapered down as the pump flow rate is titrated up to therapeutic (effective pain relief) levels over the next several weeks.
Follow up 2 weeks with neurosurgeon (October 27, 2015) after pump implantation surgery. Healing nicely.
Following picture shows wearing a binder:

Most of the swelling and bruising gone around 2 weeks post surgery:

Pictured below is 1 week (October 19, 2015) after pump implantation surgery. The swelling and bruising at the surgical site is to be expected. Pain levels high; frequent icing and wearing a binder helps.

The first pump fill was scheduled for 1 week post surgery. It was postponed by a week to allow more healing. Pump fill rescheduled for October 28, 2015.
On Monday, October 12,2015 Dr. Shehadi implanted the Flowonix Prometra II Intrathecal Pump. The pump was filled with a sterile saline solution. The first fill is scheduled for Tuesday, October 20, 2015 with Dr. Soin.
Experiencing the expected post-surgical swelling and soreness at the implant site. The pump was implanted in the same lower-left abdominal area where my previous pump was located. A small amount of additional catheter prep was needed to connect the existing Medtronic catheter with the Flowonix Prometra II pump.
Frequent icing and wearing a binder helps minimize swelling. Two Percocet 325 taken every 6 hours for pain was started on Monday afternoon then discontinued (my choice) Thursday evening, October 15, 2015.
More to follow after the first pump fill…..
Since my June 2015 update my Chronic Pain has continued to worsen. Scaling back most activities does nothing to manage the Chronic Pain. Current level of my prescribed oral opioid medication no longer even knocks the Chronic Pain Levels by one or two points.
I’ve spent a considerable amount of time learning all that is available about the new Flowonix Prometra Intrathecal Pump. I was pleasantly surprised to learn that the newest Flowonix Pump has been released and is now available. The Prometra II Pump is loaded with safety features (scroll below to review).
I reached out to Flowonix and established a relationship with their Technical Professional. He has been very helpful and informative with my questions. He even arranged for me to speak with a Flowonix Engineer in an effort to respond to my specific questions related to the Prometra II accuracy rating and safety features. My conversation with the Flowonix Engineer confirmed all the safety features the literature highlights. The Flowonix Engineer listened patiently and understood the reasons causing my low confidence in Intrathecal Pump Device Technology. By the end of our conversation I felt reassured that the Prometra II Intrathecal Pump can deliver what it claims.
Another positive indicator is that my Pain Management Doctor already has implanted the Prometra II Intrathecal Pump and the patient, thus far, is completely satisfied.
The last step in the process is to discuss surgically implanting the Prometra II Pump. My Pain Management Doctor referred me to a highly skilled Neurosurgeon. After two appointments with the Neurosurgeon along with a joint meeting with the Flowonix Technical Professional and my family, we all agreed that given my 21 year complicated history with Chronic Pain that moving forward with the Prometra II Intrathecal Pump is my best option.
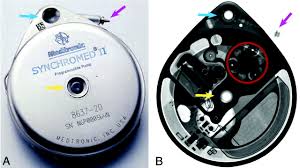
Pictured below: Flowonix Prometra II Intrathecal Pump

Pictured below: Prometra II Intrathecal Pump internal components:

Pictured below: Prometra II Intrathecal Pump seen under X-Ray

My Pain Management Doctor is certain that given my spine conditions and age, my level of Chronic Pain will continue to worsen. My only other option is aggressive medical management involving more powerful oral opioids.
Without question, more powerful oral opioids is not an option. In light of the new Flowonix Prometra II Intrathecal Pump’s advancement in key safety feature I am awaiting the surgery implantation date.
Technology has taken a key role in the management of my Chronic Pain. Click on the following link to learn about what medical implant devices I use:
mypainweb’s technology intervention
I recently learned from my Pain Management Doctor that a new Intrathecal Pump Technology has been introduced and is being implanted. The device manufacturer is a company called Flowonix located in New Jersey. The Intrathecal Pump is called Prometra.
Flowonix has created a pump delivery system which claims significantly superior infusion accuracy as compared to Medtronic’s Synchromed II pump. The reason I finally decided to have my Medtronic Synchromed II pump removed was due to the two (2) serious unexpected over infusion episodes I experienced. The growing list of Medtronic Pump problems resulting in numerous Product Advisories, FDA Recalls and impending legal action against Medtronic caused me to lose confidence in this device.
The links below will familiarize you with the serious problems plaguing Medtronic’s Synchromed II Intrathecal Pump:
Medtronic Synchromed II Intrathecal Pump Product Advisories
Medtronic Synchromed II Over Infusion Advisory
FDA Medtronic Synchromed II Recall-June 2013
FDA Files Consent Decree with Medtronic-April 2015
The additional Synchromed II Intrathecal Pump questions, accusations, and charges being filed against Medtronic citing manufacturing concerns and questionable complaint reporting/investigating practices lowered my confidence even further.
What I sorely miss is the pain relief the pump delivered when it did work as expected. This benefit, unfortunately, no longer outweighed the risks as at least 14 people have died from the same Medtronic Synchromed II over infusion malfunction that I suffered, not once, but twice.
Oral opioids have been my primary source of pain relief. The level of pain relief from my current opioid dosage no longer provides effective pain relief due to the tolerance factor associated with long term opioid use. The only option is to increase the opioid dosage or switch to a stronger opioid. I resist this tact as absorbing stronger opioids will result in potential dangerous side effects including addiction and depression.
I’ve reduced even further my activity levels in an effort to manage the pain levels. This has proven to be futile as being sedentary brings another set of frustrating side effects. Once again, mypainweb’s complication grows.
This is when having a partnership with your Pain Doctor is crucial. My Pain Doctor understands my complicated Chronic Pain history. The easy way out would be for my Pain Doctor to simply encourage me to increase the opioid dosage or switch to a much stronger opioid. Fortunately, my Pain Doctor shares my conservative and cautious approach to long term opioid therapy. His suggestion of returning to Intrathecal Pump therapy using this new technology has me initiating due diligence in learning as much as I can about the Flowonix Prometra intrathecal pump.
Without getting too technical, the main difference between Medtronic’s Synchromed II pump and Flowonix’s Prometra pump has to do with how the pump delivers the intrathecal pump medication from it’s internal reservoir. The Synchromed II pump uses a motorized gear while the Prometra pump uses pressure generated from it’s stored propellant.
Here’s a few pictures of what we’re talking about:
Medtronic Synchromed II:
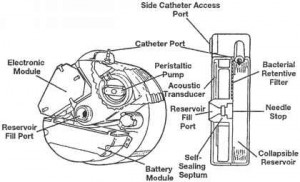
Flowonix Prometra:

Want to know more about the 2 types of intrathecal pump technologies?

Click on the following link to learn more about the Medtronic peristaltic pump (Synchromed) compared to the Flowonix valve-gated pump (Prometra):
Intrathecal Pump Technology Comparison
While I’m interested in my Pain Doctor’s suggestion of the Prometra Intrathecal Pump, we agree to carefully move in this direction. Given the relative newness of Prometra and the fact that Flowonix will be announcing a new Prometra model early next year, there is no reason to move too quickly. This will also give me time to reach out to patients that have implanted the Prometra Intrathecal Pump to get their feedback.
I will share my findings as I continue my Chronic Pain journey…..
Those with Chronic Pain will completely understand when I say it’s been “my turn”. “My turn” for experiencing several weeks of worsening pain. The increased pain creates the need to be isolated which thickens the cloud of depression. Many times the Chronic Pain sufferer can pinpoint the root cause of the prolonged pain spikes. For me, the recent surgical removal of my intrathecal pump (similar one pictured below) resulted in the return of greater pain.

Click on the link below to read why I decided to have my intrathecal pump removed:
Only one thing to do…..Take charge of “my painweb”! Wearing the molded brace shown below will hopefully help manage pain levels allowing me to resume some activity.

Many of you have been asking about my Medical Evaluation follow up since starting the Paleo Diet. The purpose of the followup was to objectively assess what effect the Paleo Diet has had on my health. My primary care physician conducted standard blood tests, checking for HDL, LDL, total cholesterol levels, and triglyceride levels.
I feel it’s important to have this type of objective benchmark in order to answer my questions: Is “Paleo right for me?” Is Paleo safe for my health? Is Paleo achieving results?. No gimmicks. No sales pitch. No baloney. No media hype.
The Paleo diet seemed the best fit for my initial objectives 5 months ago:
*Anti-inflammatory diet to help manage Chronic Pain
*Increased energy levels
*Overall general improved level of health.
Paleo was my diet selection which I started on April 21, 2014. The Paleo claims that appealed to me most included:
*Healthy lifestyle
*Clean food
*Simplicity
*Lifetime benefits
*logical research findings
Body Mass Index (BMI):
Body Mass Index (BMI) is a number calculated from a person’s weight and height. BMI provides a reliable indicator of body fatness for most people and is used to screen for weight categories that may lead to health problems.
BMI chart:
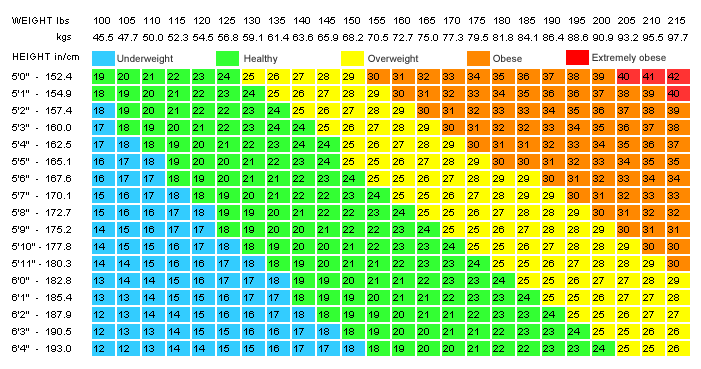
Below is my BMI comparison. The 2 point BMI improvement moves me from the “slightly overweight“ category to the “normal” category.
DATE August 31,2012 September 15, 2014
BMI 25.37 kg/m2 23.02 kg/m2
Weight 162 lb. 147 lb.
Height 5’7” 5’7”
Lipid Panel / Cholesterol:
A lipid panel is a blood test that measures fats and fatty substances known as lipids. Lipids are found in your blood and tissues. These fats are used as energy in your body, but if levels become too high and unbalanced lipids can build up in the artery walls to form plaque. This can obstruct blood flow through the arteries and increase cardiovascular disease and stroke risks. Lipids include cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), and triglycerides.
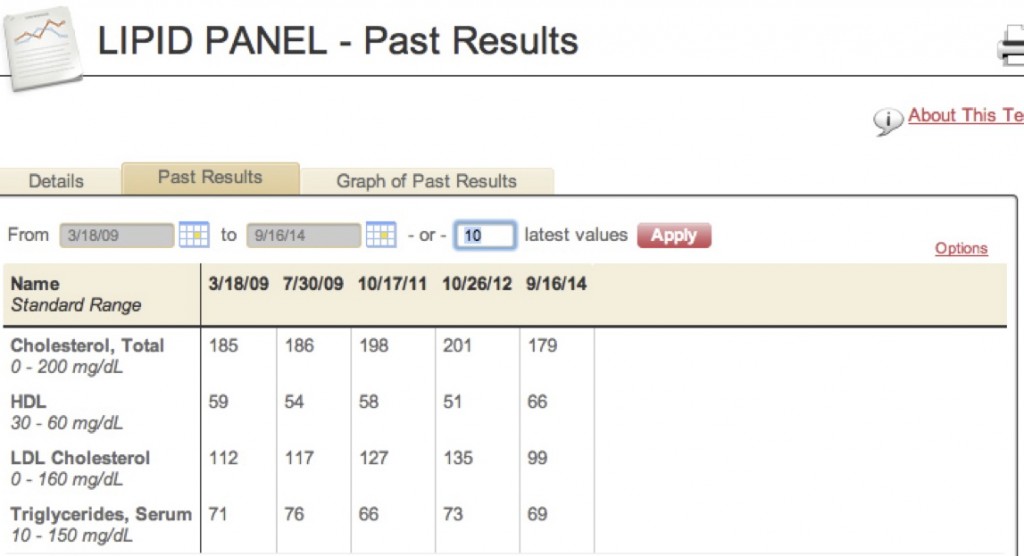
My best Lipid Panel results are from the latest 9/16/2014 which illustrates the positive impact Paleo is having on this key measurement. High cholesterol levels are notorious within my family due to genetics. Severe arteriosclerosis and heart disease run high on both sides of my family causing added concern. Though a 22 point decrease in my total cholesterol count (9/16/14 vs 10/26/12) may appear modest, it’s actually a substantial improvement.
Lipid Panel Standard Range Reference Guide:
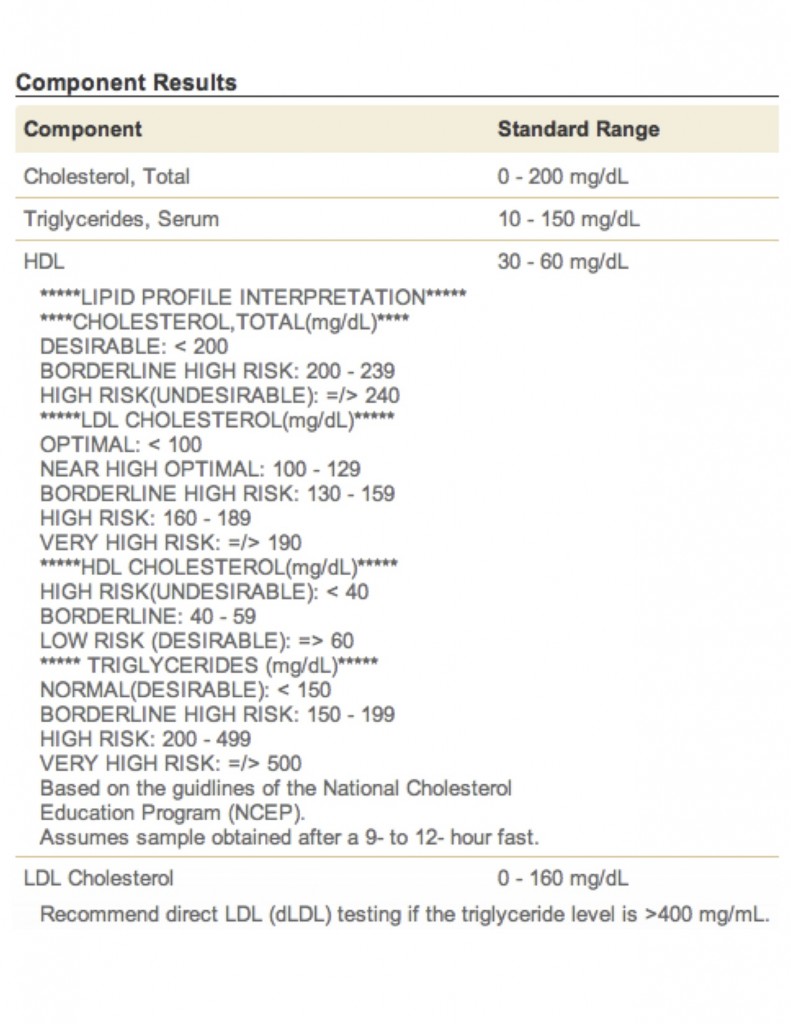
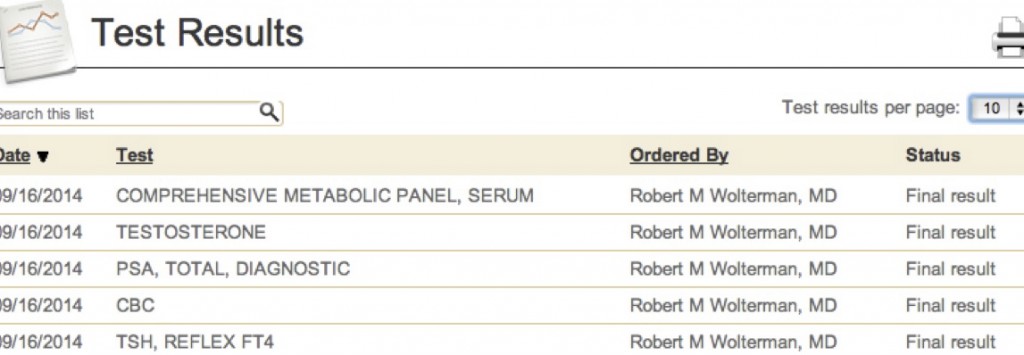
Additional tests:
The following additional tests were also performed. All results fell well within “normal” ranges.
Given the extensive length of these tests, I will be happy to furnish these test results upon request. Email your request to help@mypainweb.com.
Is this a guarantee of results that the Paleo Diet will have for all? No. But it does warrant your serious consideration of Paleo if you seriously want to achieve a healthy body weight with desirable cholesterol levels along with other key health benefits.
In the midst of all the promises and claims advertised and promoted by celebs and slick campaigns of many diet programs, my Paleo feedback offers simple, truthful results.
Overall, I am satisfied with Paleo. Following the Paleo Plan has met my initial objectives set 5 months ago.
Benchmarking the aforementioned medical diagnostic testing helped me satisfy and establish objective measurements while creating some “Paleo confidence”.
I will continue to share Paleo Updates as I continue to “Go Paleo”.
Paleo still trending just past the 18 week mark. Why continue??
During one particular “mealcation” (earned brief break from Paleo), I ate a number of “healthier” food items; selections I used to eat on a regular basis before Paleo. Tortilla chips & salsa, pasta, cheeses along with a beer finishing with Ghirardelli brownies during a Labor Day dinner celebration with friends.
Man, everything tasted awesome; a few of my former comfort foods. Overall, I could have picked far worse items to eat for my Paleo “mealcation”.
Several hours later I noticed the ring on my finger was snug and I felt noticeably warm. The warm sensation was not like a fever, but a peculiar “warming” along with feeling almost “flush”. Accompanying the above was distinct thirst.
Without question, I was experiencing the classic “inflammation” response to the “mealcation” foods I ate as these items are ranked “high” on the inflammatory foods list. Upon resuming my Paleo foods, the inflammatory response (swollen, warm, flush) was gone.
In my opinion, Paleo works by eating healthier and cleaner. Removing the inflammatory response our bodies have to sugar, food chemicals & additives, high glycemic carbs along with other Paleo principles does make a difference.
Soon, I will have a lipid panel done to compare “before and after” cholesterol levels prior to starting Paleo on April 21, 2014 to present. HDL-LDL comparisons will be a key marker to gauge objective Paleo Results.
In the meantime, motivation to continue Paleo remains high.
Low Carb Beats Low Fat for Weight Loss, CV Risk
A recent study reports that cutting down on carbohydrates was a more effective strategy than limiting fat intake for weight loss and for reducing cardiovascular risk in a randomized trial, researchers found. This approach is very similar to the Paleo Diet.
Click on the following link to read the recent study findings:
Low Carbs Beat Low Fat for Weight Loss, CV Risk
The following article supports a Paleo-like diet as it further dispels traditional core nutritional beliefs & values:
Paleo going strong at the 11 week mark. How’s it going you ask??
Let me first revisit the reasons for going Paleo:
1. Greater pain management control through a Paleo diet’s anti-inflammatory effect
2. Reduce intake of food chemicals & additives
3. Increase energy levels with improved mood & outlook
4. Obtain improved health via burning fat for energy versus burning carbohydrates
5. Maintain ideal bodyweight without counting calories
How do we “grade” the Paleo diet?
While at first glance the above Paleo “grades” may be somewhat “unimpressive”, there is a very tangible feeling of health & satisfaction by eating “clean” foods that contain no chemicals and laboratory created additives & modifiers. Combining this with the above “grades” results in a resounding YES to continue Paleo.
Here are a few “sidebar” comments:
Your shopping and food preparation habits do change in the beginning as I mentioned weeks earlier. Don’t fret as this process get’s easier as you settle in with your favorite Paleo menu items & snacks.
Yes I did mention “snacks”. Snacks are important!! One of our Paleo favorites are any kind of berry; either by themselves or in a smoothie. Needing something more substantial that you can really “sink your teeth into”? Try the Paleo friendly Larabar Bar.
Click on the following link to learn more about them: Larabar Bar

Even better…..check out Laura’s own Paleo Bar recipe below. Fast, easy, satisfying & completely Paleo legal!

Laura’s Paleo Bars:
Ingredients:
1. 1 cup raw nuts
2. 1 cup pitted dates (no sugar added)
3. 1 cup dried fruit (no sugar added)
Steps:
1. Blend all the above in food processor
2. Press into 8″x8″ pan lined with wax paper
3. Refrigerate till firm
4. Cut into 1′ to 1.5″ squares & store in airtight container in refrigerator
Add some of these ingredients for awesome combo’s:
1. walnuts, dates, golden raisins and, or Goji berries adding organic unsweetened coca powder & fresh ground expresso beans
2. pecans, dates & dried cherries
3. almonds, Goji berries & dates
4. try different combinations!!
Paleo bars not decadent enough to hit that “sweet spot”? Scroll to down to Laura’s Paleo-friendly chocolate cake. Guaranteed to do the trick!
“Feed the need” and reach for a crunchy snack?? Try Brads Raw Chips with guacamole….a super Paleo snack (yes, avocados are completely Paleo legal). Brads Raw Crunchy Kale is a tasty Paleo snack too.
Click on the following link to find out about the complete Brad’s Raw product line up:
Sure we’ve had a few Paleo “stall” moments. That’s where the “mealcation” works. It’s OK to have a non-Paleo food item “vacation” once-in-a-while as a reward. Go ahead and have a slice of pizza or burger with the “works”. Just be sure you keep the “mealcation” under control.
Dining out has gotten much easier too. We have a pretty good handle on what food establishments are better suited for Paleo ingredients. Most servers are more than willing to accommodate our Paleo palate too!
Just one day shy of going Paleo for 6 weeks. I’ll share a few observations and results:
* Without question, it’s not a diet of “convenience”. However; the routine is easy provided you preplan meals & fine-tune food shopping habits.
* There is a very real & tangible feeling from eating “healthy” foods.
The process of digesting a complete meal prior to Paleo made my abdomen feel full/extended for sometime as the process of digestion took time. On Paleo, that full feeling is absent and the process of digestion takes much less effort & takes much less time.
* The usual periods of feeling added fatigue during the afternoon seem to be wearing off. I had thought this fatigue was a result of my natural 24 circadian rhythm. I now believe that this fatigue was most likely related to my glycemic levels spiking & falling from the foods I was eating.
The anti-inflammatory effect of Paleo was my main goal to help me manage my Chronic Pain. A fair assessment of Paleo on my Chronic Pain will take more time. The recent surgical removal of my intrathecal pump has my body continually adjusting to this significant pain management change. The elimination of intrathecal pain medication while increasing oral pain medication will take a longer period of time to gauge anti-inflammatory impact.
I prefer solid “measurements” to compare before & after Paleo. I will follow up with obtaining a post-Paleo lipid panel to compare with previous lipid panels done prior to going Paleo. I am curious how Paleo affects my LDL/HDL cholesterol numbers. Given my body is now, in theory, burning fat as opposed to burning carbohydrates, it will be interesting to see the net cholesterol change. Weight loss was not a goal of mine, so I’m not motivated to monitor this measurement. Paleo does advocate more “healthy fats”, so I will report on this topic more over time.
Overall, my wife, Laura, and I continue to be motivated by Paleo. We have done a good job of finding “paleo-friendly” alternatives to most of our pre-Paleo comfort foods. We’re also encouraged to discover more and more people we know turning to “Paleo”, or seriously considering “Paleo”.
Get “Fed-Up” with the help of mypainweb.
Here are some of the sobering facts about the state of health in America revealed in “Fed Up,” a new documentary from producers Katie Couric and Laurie David about the country’s food industry: (1) “Over 95 percent of all Americans will be overweight or obese in two decades”; (2) “By 2050, one out of every three Americans will have diabetes”; (3) 80 percent of food items sold in America have added sugar.
HuffPost Entertainment has debut the new poster for “Fed Up,” which is out in theaters on May 9, 2014:
The film’s official synopsis and must-see trailer are below:
For the past 30 years, everything we thought we knew about food and exercise is dead wrong. FED UP is the film the food industry doesn’t want you to see. From Katie Couric, Laurie David (Oscar winning producer of AN INCONVENIENT TRUTH) and director Stephanie Soechtig, FED UP will change the way you eat forever. The film opens in theaters across the country on May 9, 2014.
Click this link to watch the official trailer:
In the past ten years, researchers have found a solid link between sugar consumption and inflammation. Spikes in blood sugar levels promote inflammation and inflammation leads to chronic pain. – See more at: Sugar leads to Spike in Chronic Pain
The American Journal of Clinical Nutrition reported that processed sugars and other high-glycemic starches increase inflammation, which causes pain, overheating, redness and swelling. Click the following link for more details: When food causes you pain
Review some research for yourself: AJCN
GMOs, or “genetically modified organisms,” are plants or animals that have been genetically engineered with DNA from bacteria, viruses or other plants and animals. These experimental combinations of genes from different species cannot occur in nature or in traditional crossbreeding.
Most developed nations do not consider GMOs to be safe. In more than 60 countries around the world, including Australia, Japan, and all of the countries in the European Union, there are significant restrictions or outright bans on the production and sale of GMOs. In the U.S., the government has approved GMOs based on studies conducted by the same corporations that created them and profit from their sale. Increasingly, Americans are taking matters into their own hands and choosing to opt out of the GMO experiment.
In the U.S., GMOs are in as much as 80% of conventional processed food.
Concerned about GMO’s? Read all about GMO’s and what you can do about it by clicking the following link: GMO’s
What to do??
The facts are overwhelming that support what I choose to eat will affect my Chronic Pain and overall health.
I chose the Paleo Diet as a way to help gain more control of over my Chronic Pain and help to improve my quality of life.
Laura and I took our first “mealcation” yesterday. What the heck is a “mealcation”? The MaximizedLiving Paleo Diet encourages an occasional reward in the form of giving oneself a “break-from-Paleo”. Our “mealcation” was enjoying a fat, juicy delicious burger with condiments!! The meat was Pale0-friendly, but the bun and condiments were loaded with chemicals & sugar. Wow…..did it ever taste awesome. A well-deserved prize for staying strict with Paleo for 23 days.
Paleo is no longer a chore, but rather the choice we want to continue with. As cliche as it may sound, there is a positive return in the form of a “feeling” which comes with being chemically liberated from unhealthy foods. Laura is continuing to lose modest weight with a noticeable change in her body composition….a leaner; healthy look.
How are things within my Chronic Pain department you ask? While I’m still unable to report back any change in pain as a result of Paleo. I remain confident that it’s due to the post surgical pain from my May 8, 2014 Intrathecal Pump Removal Surgery. By the end of the week the surgical site should show reduce pain & inflammation with the sutures being removed this Friday, May, 16, 2014.
Look for my next Paleo update by the weekend.
We found a few Paleo-friendly menu items that are real lifesavers.
The first is a sweetener for coffee and recipes calling for a sugar/sweetener. It’s called Yacon.
Read about Yacon at the following link: Sweeteners
This gem of a sweetener does the trick without any odd aftertaste and is available on Amazon at the following link: Yacon

By now you realize most chocolate is not Paleo-friendly. Well my friends…..rejoice as Laura found this incredible chocolate Paleo-friendly dessert adding her own Paleo-friendly secret making this item “decadent & satisfying”:

Here’s the easy recipe:
Chocolate Paleo Snack Cake Recipe
Ingredients
Instructions
Alternative method for baking: Use a 9-inch round cake pan. Grease the pan and cut out parchment paper to fit the bottom. Cook per instructions above. Allow the cake to cool for about 10 minutes and turn it out onto a wire rack or cake plate to cool. Top with frosting, if desired, and cut into wedges. We’ve used whipped coconut cream and whipped dairy cream with fresh raspberries.
If you are looking for a dairy-free alternative you should try the Avocado Chocolate Frosting!
Avocado Chocolate Frosting Ingredients
Instructions
Place all three ingredients in a food processor and mix together, stopping to scrape down the sides once or twice. Stir in the chocolate chips (if using). The frosting is ready to spread immediately but you can refrigerate if you think it needs to firm up. Add a little water if it is too thick. (We didn’t need to add water)
Makes enough frosting for one single layer cake.
It’s been almost a week since we transitioned from the Advanced Plan to the Core Plan. The food items and subsequent increase in menu options give us more flexibility.
We have uncovered several Paleo substitutions for items like a Paleo-friendly sweetener for coffee and an awesome Paleo chocolate dessert! We’ll be sharing our Paleo Menu discoveries as well.
Laura remains highly motivated with some continued weight loss. My reason for going Paleo was due to it’s potential to impact my chronic pain through it’s inherent anti-inflammatory affect. The surgery to remove my intrathecal pump was performed on May 8, so pain levels are elevated due to the surgical incisions. I will discuss how Paleo is affecting my chronic pain levels when I’m further along in the post-surgery healing process.
During the first 14 days of the MaximizedLiving Paleo Diet we followed the Advanced Plan which is highlighted below:
The Advanced Plan can be used for short-term management of weight, disease, or detoxification, or may be used on a long-term basis for those who are genetically suited for it. The Advanced Plan has been researched and formulated to maximize your body’s full potential for health, energy, recovery, and cognitive power. It is designed to reduce inflammation, restore cell membrane function in order to aid detoxification, regulate hormones, and promote the use of fat (instead of sugar) as the body’s primary source for energy.
Some indications you may need this plan are as follows:
*Cognitive dysfunctions – including ADD/ADHD and Autism Spectrum Disorders
*Metabolic syndromes – including Obesity, High Cholesterol, High Triglycerides, High Blood Sugar (or Low Blood Sugar), High Insulin, High Blood Pressure, Heart Disease, and/or High Leptin
*Modern-day Illnesses – including Chronic Fatigue Syndrome, Toxicity, Fibromyalgia
*Immune System and Inflammatory Diseases – Cancer, Autoimmune Diseases, Digestive Dysfunction, Intolerance to Grains, Asthma, Arthritis
Three Rules on the Advanced Plan:
Follow the 3 Principles of the Core Plan along with the following modifications:
Fat – Increase your intake of healthy fats.
Protein – Moderate your intake of protein.
Carbohydrates – Eliminate all grains, sugars, and most fruits.
The Advanced Plan is specifically designed to eliminate cravings (something that many diets fail to do). As a result, people see dramatic results in very little time on the Advanced Plan.
So far we are encouraged and motivated to continue with the MaximizedLiving Paleo Diet. Days 4-6 were filled with some angst as we experienced some stress as we coped with “cravings” for our usual fare. We were never discouraged as the Advanced Plan food options were more than adequate. Without the need for “counting calories” the amount of food was a non-issue.
Beyond day 6 the food “cravings” disappeared. This gave us the motivation to continue through the Day 14 Goal. You will recall that one of the primary goals of Paleo is to follow the Advanced Plan so that our bodies shift gears from burning carbohydrates to burning fats.
On Day 14 our assessment of Paleo was positive. Our menu planning, food purchasing & food preparation were comfortably aligned within the Paleo Advanced Plan. In addition to no longer experiencing “cravings”, Laura began recording modest weight loss. Even more encouraging was Lauras’ ability to exercise without experiencing her usual exercise-induced-headaches & “faint’ sensation during her usual exercise routine.
We decided to transition from the Advanced Plan to the Core Plan which is suggested by MaximizedLiving.
The highlights of the Core Plan are as follows:
This plan is for everyone. The three core nutrition principles are the foundation for the Nutrition Plans, regardless of age, gender, genetic background, or medical history. Following this plan results in healthy, thriving families.
The 3 Principles of the Core Plan:
Fat – Healthy Fats vs. Damaged Fats: Eat more healthy fats and eliminate all damaged fats.
Protein – Naturally Raised vs. Unnaturally Raised Animals: Go organic and natural for all animal products.
Carbohydrates – Whole Carbohydrates vs. Refined Carbohydrates: Eat more vegetables, and eliminate refined grains & sugars.
The next update will include how we fare from the Advanced Plan to the Core Plan.
I recently made the decision to have my implanted intrathecal pump removed as I’ve experienced some serious device-related performance problems resulting in pain medication over-infusion. The loss of this advanced pain therapy leaves me with a void in my pain management control. Without question, when intrathecal pumps perform as expected they do provide some pain relief. My first intrathecal pump was implanted over 12 years ago. Since that time I experienced several periods of ups and downs. Periods of pain relief were always followed by periods of device and, or pump medication complications and setbacks. Unfortunately, this latest potential intrathecal pump problem, as reported by the device manufacturer, is the last in a series performance/reliability problems during the past few years that poses a question of risk with this technology. In my mind, and in my personal opinion, this risk which may result in death, far outweighs the benefit of some pain relief.
I became motivated to aggressively continue searching mypainweb for pain relief from the absence of relief I now experience without the intrathecal pump. The obvious solution of increasing oral opioid medications is not an option. Visit mypainweb.com to read “Opioid Truths”.
It didn’t take long for me to understand that what goes into my body will either hurt or help me. Nutrition and the proven link of the inflammation-response cycle of what we eat was an obvious answer as a pain relief strategy. Visit mypainweb.com to read my initial Chronic Pain Diet and Nutrition section.
There are a number of foods that, when eaten regularly, result in a vicious cycle that promotes pain. These foods irritate pain sensitive nerves and promote the production of several substances that increase the body’s inflammatory response. In addition, these foods can interact with part of your intestinal tract in a way that results in what is called intestinal permeability, or more commonly, leaky gut, which can further promote inflammation (as well as a host of other problems).
The inflammatory process is the body’s response to injury. Its main purpose is tissue healing and protection of your health. For example, if your skin is scratched and bleeds, even a tiny bit, your immune system responds to fight off any unwanted bacteria from outside your body. Part of that response is inflammation which is a cascade of molecular, cellular and biochemical processes. This is true for injuries, large and small, as well as normal daily wear and tear. Inflammation is designed to be a beneficial process. Problems arise when inflammation is excessive, out of proportion to an injury or present for undiscovered or unknown reasons.
How does this relate to food? Your body’s inflammatory response is upset when you eat a diet that is deficient in fruits and vegetables (which are anti-inflammatory) and instead eat excess sugar and simple starches (breads, cakes, cookies, potatoes), vegetable and seed oils (soybean, corn, safflower, peanut, cottonseed), trans fats, and go overboard on saturated animal fat (particularly from sedentary, obese, industrially raised cattle, chicken and pigs). This all too common diet generally will not cause immediate symptoms but eventually, diet-driven inflammation can lead to chronic aches, pains and many other health problems. As I stated earlier, if you eat mostly vegetables and fruits and meat from animals that ate their natural diets, the management of chronic pain and inflammation becomes far easier.
As a bonus, people who eat in this Paleo Diet manner usually lose weight effortlessly, have better cardiovascular health, improve blood sugar readings and report greatly increased energy. Click on the following link to read more: Reducing Pain and Inflammation with Diet
Each organ, and even the bloodstream, contains a part of our immune system, which uses inflammation to protect us from bacteria, viruses, parasites, molds and foreign proteins as well as to heal wounds. Ideally, such threats are neutralized and the associated inflammation is resolved.
An unresolved inflammatory response (chronic inflammation), however, can spread damage throughout the body. Researchers from different areas of medicine have independently and repeatedly concluded that inflammation plays a key role in a variety of illnesses.
Those who claim to have tried everything in pursuit of chronic pain relief, addressing underlying pro-inflammatory dietary practices can be a fundamental key to recovery. The Paleo Diet can be the key that unlocks the door to sustained pain relief.
The principles of the Paleo Diet are valuable as it is essentially an anti-inflammatory diet. For instance, chronic pain sufferers who attempt to combat symptoms without addressing underlying omega-3 versus omega-6 imbalances from over reliance on grains and lack of animal sources of DHA and EPA, are fighting an uphill battle. The same can be said for foods with high glycemic indices that also have a pro-inflammatory effect. Click on the following link to read more: The Paleo Diet is an anti-inflammatory diet
There’s no question that what we put in our mouths — and how much of it — has a big influence on our health. But no one diet has been shown to prevent inflammatory-linked diseases.
The problem is that the majority of studies linking diet to disease either are too small or are retrospective — that is, they ask people what they ate in the past and then try to correlate that to their current-day health. And studies have shown that people don’t accurately recall what they’ve eaten in the past.
A proper study includes a prospective, randomized, placebo-controlled, double-blind study which takes two groups of similar people, some eating normally, and others eating an anti-inflammatory diet, and compares the changes in their health over time. And the entire time, neither the doctors nor the patients know which diets they’re on. It’s the way most pharmaceutical drugs are evaluated, but studies looking at diet or nutritional supplements are rarely held to this standard.
While there’s no hard, evidenced based proof that anti-inflammatory “cures” anything, it’s important to emphasize anti-inflammatory diets not bad, but Chronic Pain sufferers shouldn’t expect a miracle cure. Click on the following link to read more: Can Diets Fight Chronic Pain? The Science Isn’t There
Eating badly or not enough can have significant consequences, leading to a loss of energy, fatigue, stiffness, a reduction in activity, and feelings of discouragement. Any of these can increase the severity of pain. Click on the following link to read more: NUTRITION & CHRONIC PAIN
Recent data suggests that central sensitization, in which neurons in your spinal cord become sensitized by inflammation or cell damage, may be involved in the way fibromyalgia sufferers process pain.
Certain chemicals in the foods you eat may trigger the release of neurotransmitters that heighten this sensitivity. Click on the following link to read more: Foods That Chronic Pain Sufferers Need to Avoid
It may be that the foods you eat render your chronic pain worse, or better. Only the one who eats is the one who will know whether a given diet improves chronic pain.
Click on the following link to read more: Nutrition and Chronic Pain
What did I decide to do?

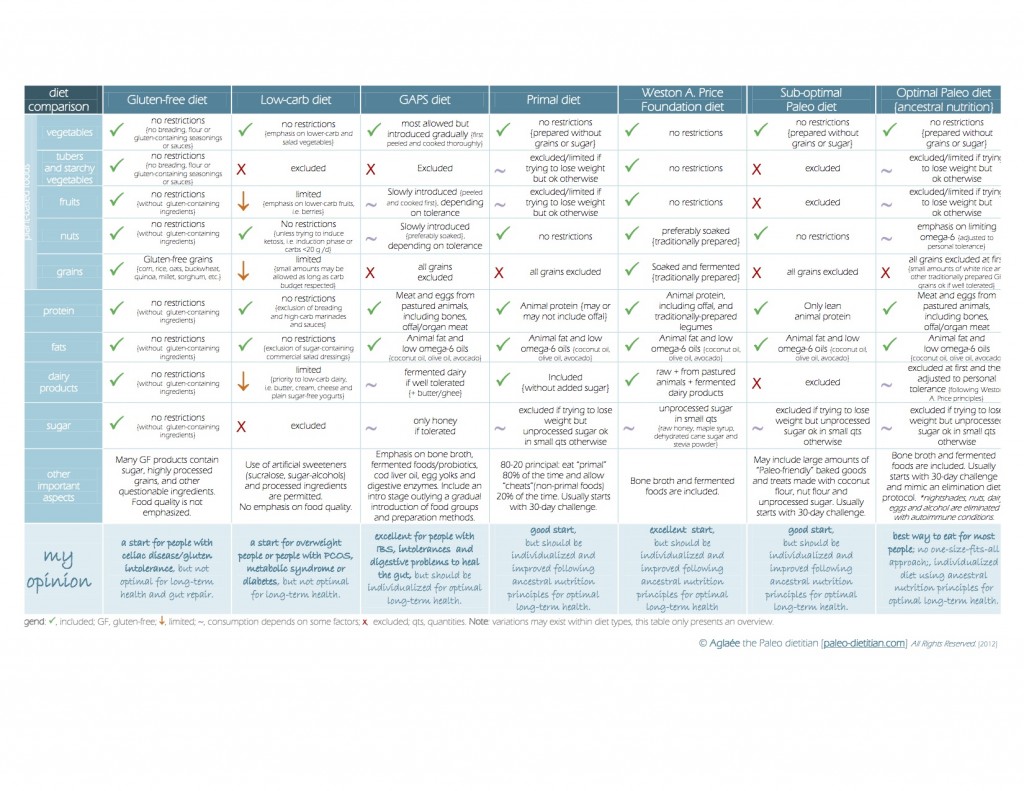
The following chart shows the various nutrition plans & diets compared:
On Monday, April 21, 2014 Laura, my wife, and I started a Paleolithic diet, also know as a Paleo diet. While there are many Paleo diets, we chose The Maximized Living Nutrition Plans.
Ten years ago sugar wasn’t even on the radar as a harmful substance. Back then, health officials weren’t thinking about the significance of sugar consumption and its serious effect on our body. Since then, we’ve seen dramatic changes in the world of health and we now know sugar’s impact on our internal system. More and more individuals are showing interest in eating better; they’re eliminating sugar and including whole, organic, non-processed foods in their diets. The Maximized Living Nutrition Plans were born from this movement in 2009. Now, several individuals still have a lingering question: “What is Paleo? And is it a good choice for me?”
A Paleolithic diet is made up of whole, unprocessed foods — largely meat and vegetables with a limited amount of fruit and nuts and no grains or sugar (basically, anything that can be hunted or gathered). “Paleo”, or the Paleolithic diet, can be confusing. In her article, Seven Shades of Paleo, Amy Kubal speaks to the murkiness around what it means to be Paleo and reviews several classifications of a Paleolithic lifestyle. Generally, individuals who choose a Paleo diet cut carbohydrates and processed sugars, but because there are so many different styles of Paleo, it’s difficult to precisely define. In fact, because the terminology has become so popular, it is my opinion that there isn’t a diet more ambiguous, yet so widely followed.
The Paleo movement was first popularized in the mid-1970s when a gastroenterologist named Walter L. Voegltin promoted a very primal way of living. His nutrition plan encouraged eaters to consume grass-fed pasture meats, fish, vegetables, fruits, nuts and exclude grains, refined salts, refined sugars, processed oils and dairy products, because, according to Voegltin, our ancestors ate this way and were able to sustain their health for a much lengthier period of time than we do today. People like Loren Cordain and Dr. Ron Rosedale who promote the “caveman diet” argue that people in the Paleolithic era thrived on such a diet and would never have consumed grains because there was no form of agriculture in that time period. The accepted Paleo framework laid out by Voegltin diet is a step in the right direction, and the Maximized Living Nutrition Plans provide clarity in the application of Paleo principles.
Click on the following link to learn more about The Maximized Living Nutrition Plans: MaximizedLiving
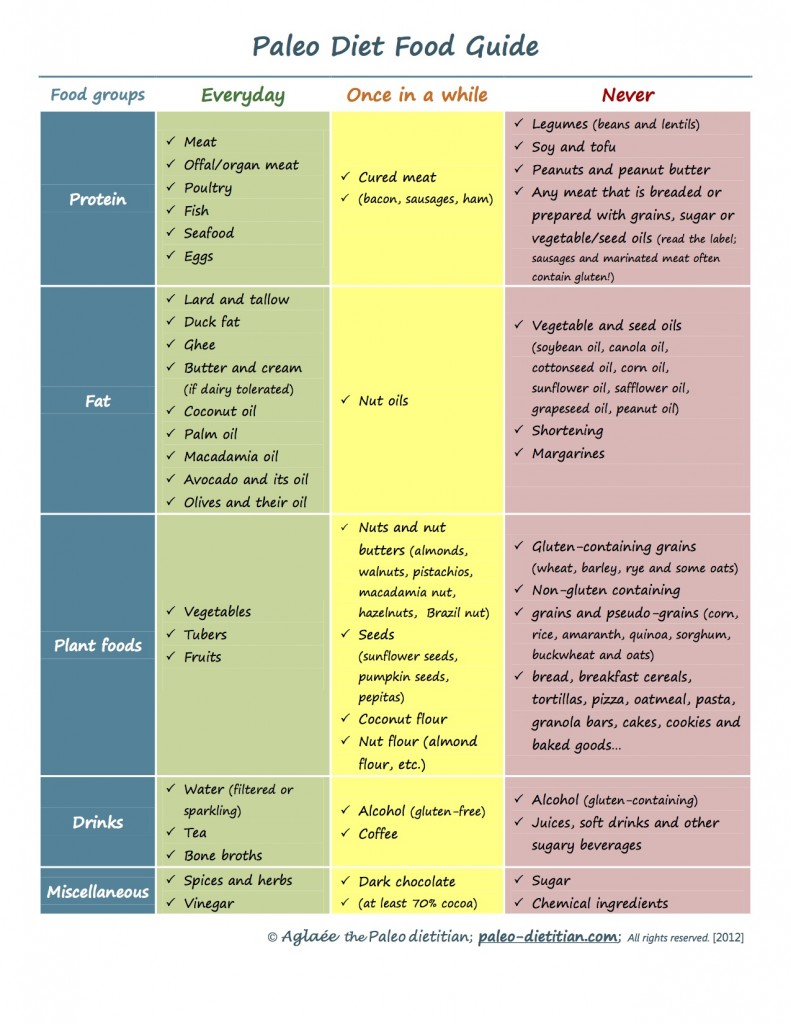
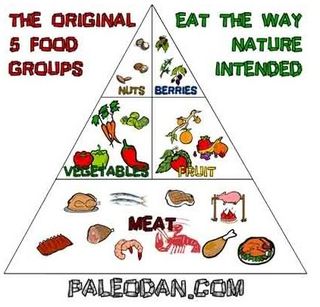
The following shows the Paleo diet seen in our familiar food triangle:
The first 10-14 days involve a strict adherence to the Maximized Living Advanced Plan. It is during this initial phase that the body will change from burning carbohydrates to the healthier method of burning fat.
I will share my experiences in the days,weeks, and months ahead on mypainweb.com/blog.
While I don’t know what pain relief, if any, I will experience I do know that making the decision to change my eating to a Paleo Nutrition lifestyle is another way to control mypainweb and improve my quality of life.
It was but a few seconds in time, that accident in 1994 that changed my life forever. While at the gym, the Cybex Lat Pull Down machine failed while I was using it, which caused a severe low back injury. A multi-level spinal fusion surgery with implanted instrumentation (hardware) was required to repair the damage. After several months of physical therapy I was able to return to work. One fateful day not long after my return to work I was attending a meeting. While seated around a boardroom table with some of my colleagues, the chair I was sitting in broke, causing me to fall onto the hardwood floor. The point of impact was the site of my spine fusion. The impact caused further damage to my spine. A second, multi-level spinal fusion surgery with hardware was required to repair the damage. Intense physical therapy followed, and I was once again able to return to work. Though my orthopedic surgeon cleared me to return to work, my employer refused to reinstate me. Instead, they offered me a lesser position in another state, which would require me to relocate. Instead, I decided to seek employment elsewhere. During the following two years the damage to my spine continued to worsen. A third spinal fusion surgery with hardware was required. Despite intense physical therapy I was unable to again return to work.
The effects of the chronic pain along with limited function and mobility has slowly changed me. Over time, depression set in, as I sought to find appropriate treatments to return me to the individual I once was. The motivated, outgoing, positive, executive level manager was changed into a depressed, withdrawn, irritable individual, unable to work while coping with disability.
Despite several additional surgical procedures, the chronic pain continued to worsen. Years of pain medication usage further changed me as I attempted to manage the pain. The result was further medical complications, greater pain, and a loss of quality of life.
My role as husband and father was also affected. My inability to play with my kids and be the husband my wife married, along with the inability to earn a living, deepened my depression and despair.
Hiding my pain and pushing away those who loved and cared about me was my existence. It was clear to me that my best days were behind me.
Years later it became apparent to me that my chronic pain was permanent. It could not be healed. I had two options: continue to allow the pain to control me, or take charge and control the pain. If I wanted to live, the latter was my only choice.
mypainweb blog shares with you my journal of my chronic pain.
mypainweb.com is my website which shares with you how chronic pain took control of every aspect of my life. Once I realized this, it was a step in the right direction. Am I the individual I once was? No. Do I still suffer from chronic pain? Yes. Will I face more surgeries and medical treatments? Most likely. The difference now is that I understand I must take charge and control mypainweb. Rather than continuing to close myself off from the world I’ve begun talking about my chronic pain journey. I’ve begun to reach out to others in an effort to help them face their own chronic painweb.